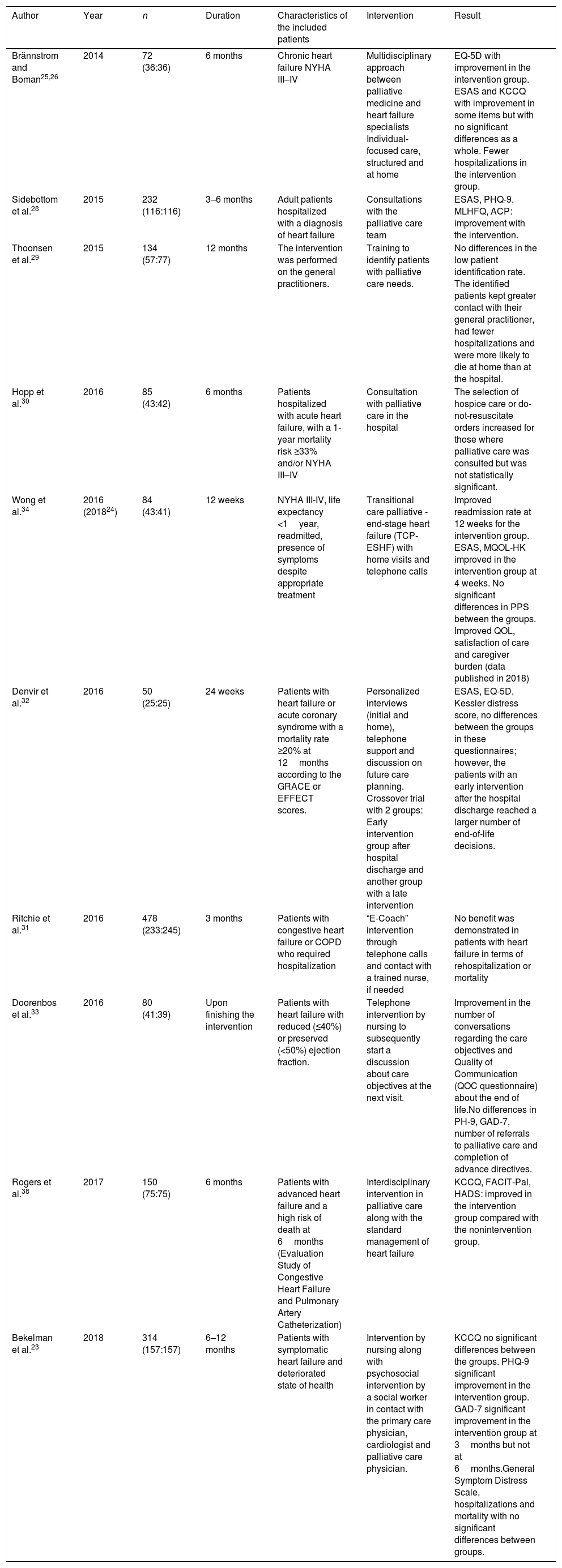
Although heart failure is one of the most common clinical syndromes in medicine and has a high mortality rate, few patients have access to adequate palliative care for their clinical situation. Several trials have recently been published on the usefulness of starting palliative treatment along with cardiac treatment for patients with advanced heart failure. In this review, we analyze the aspects of diagnosing and controlling the symptoms of patients with advanced heart failure and provide a collection of clinical trials that have analyzed the efficacy of a palliative intervention in this patient group. Physicians need to be equipped with strategies for recognizing the need for this type of intervention without it resulting in neglecting the active treatment of the patient's heart failure.
A pesar de que la insuficiencia cardiaca es uno de los síndromes clínicos más frecuentes en medicina y de su elevada mortalidad, pocos son los pacientes que se benefician del acceso a unos cuidados paliativos adecuados a su situación clínica. Recientemente se han publicado varios ensayos para comprobar la utilidad de iniciar tratamiento paliativo junto con el tratamiento cardiológico en pacientes con insuficiencia cardiaca avanzada. En la presente revisión se analizan aspectos sobre el diagnóstico y el control de síntomas de pacientes con insuficiencia cardiaca avanzada, y se ofrece una recopilación de ensayos clínicos que analizan la eficacia de una intervención paliativa en este grupo de pacientes. Es preciso dotar al médico de estrategias para reconocer la necesidad de este tipo de intervenciones sin que ello implique descuidar el tratamiento activo de su insuficiencia cardiaca.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<