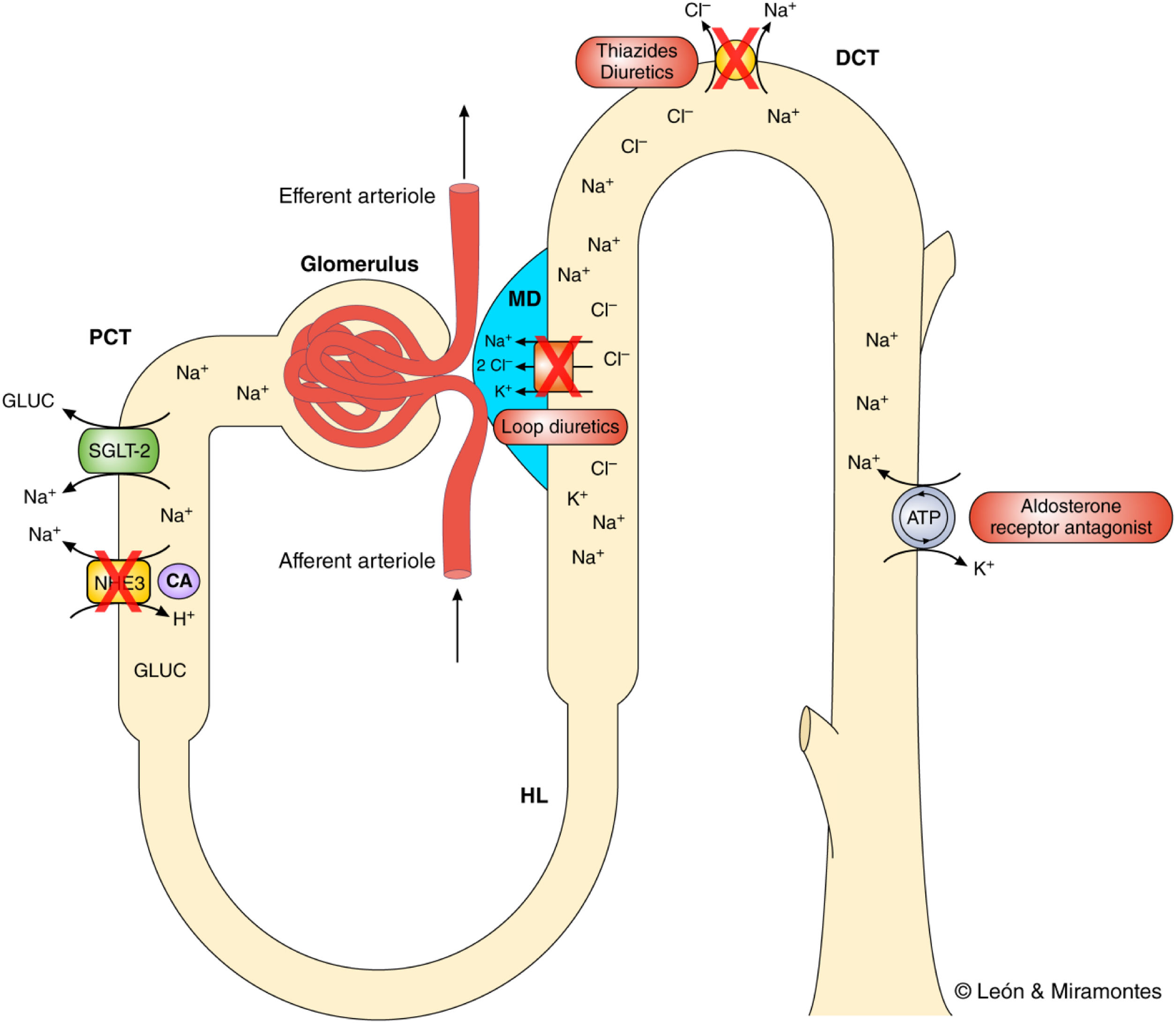
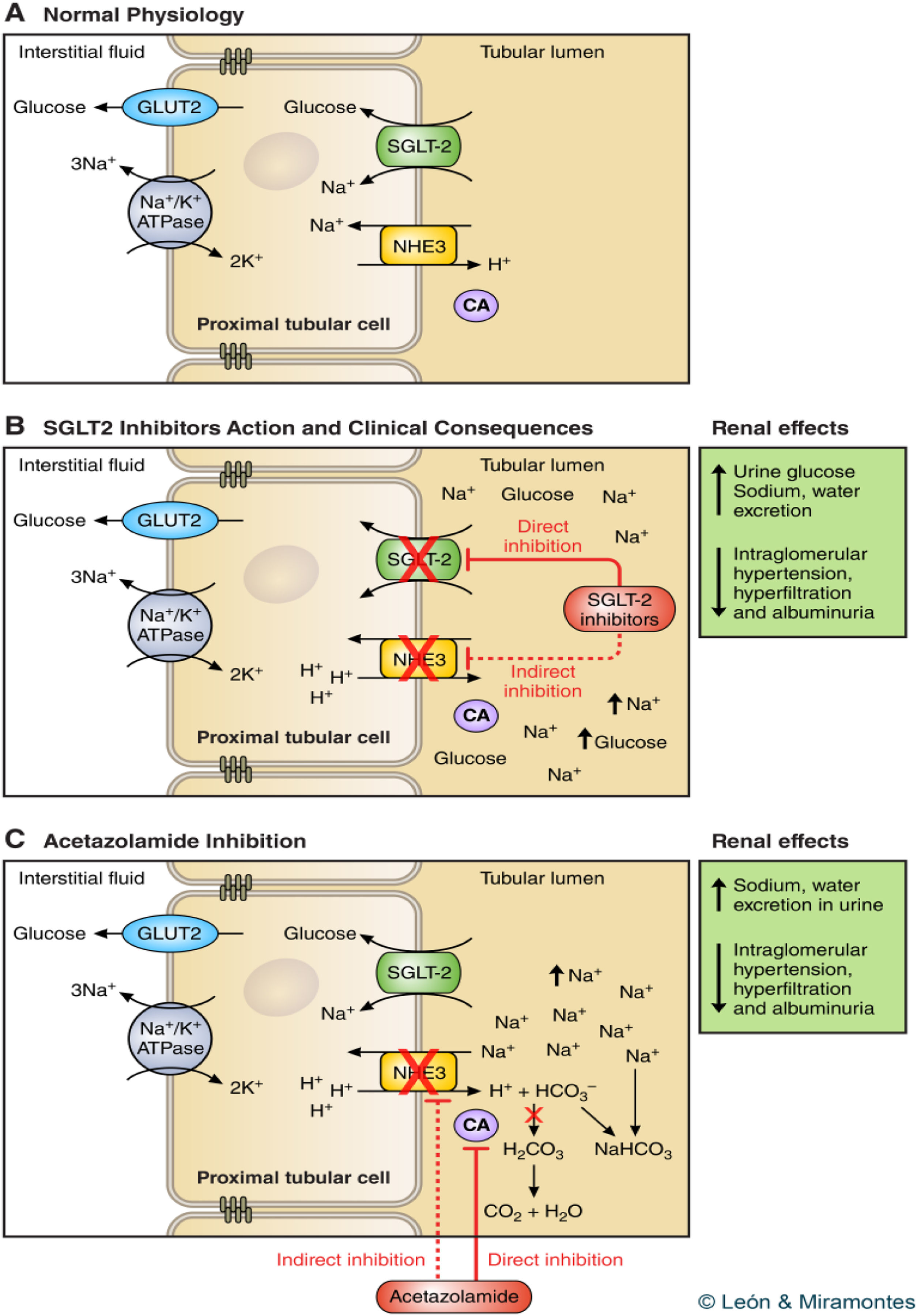
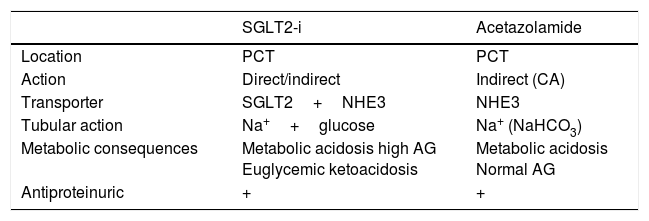
Sodium-glucose cotransporter-2 inhibitors have changed the concept of the effects that hypoglycemic drugs have on hearth failure (HF). For the first time, a therapeutic group has modified the evolution of HF. Its effect goes beyond glycemic control, and different theories have been postulated to justify this benefit. In the article we sent, we analyze the influence of the different pharmacological groups used in type 2 diabetes mellitus on HF, and we present the theory of the mechanism of action associated with the benefit of these drugs. In our opinion, this benefit in HF is secondary to its diuretic effect, specifically an effect very similar to carbon dioxide inhibitors.
We think that our theory is novel, explains the mechanism of action and we have not found in the literature any article that explains the mechanism of action in such a precise way.
Los inhibidores del cotransportador sodio-glucosa tipo 2 han cambiado el concepto que se tenía de los efectos que ejercen los fármacos hipoglucemiantes sobre la insuficiencia cardiaca (IC). Es la primera vez que un grupo terapéutico modifica la evolución de la IC. Sus efectos trascienden al control glucémico, postulándose diferentes teorías para justificar estos beneficios. En este artículo analizamos la influencia que tienen sobre la IC los distintos grupos farmacológicos utilizados en el tratamiento de la diabetes mellitus tipo 2, y planteamos el posible mecanismo de acción asociado con los beneficios aportados por estos fármacos. Somos de la opinión de que este beneficio sobre la IC es secundario a su efecto diurético, en concreto a una actividad muy parecida a la de los inhibidores del dióxido de carbono.
Pensamos que se trata de una teoría novedosa que explica el mecanismo de acción. No hemos encontrado en la literatura ningún artículo que desarrolle de manera tan precisa dicho mecanismo.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<