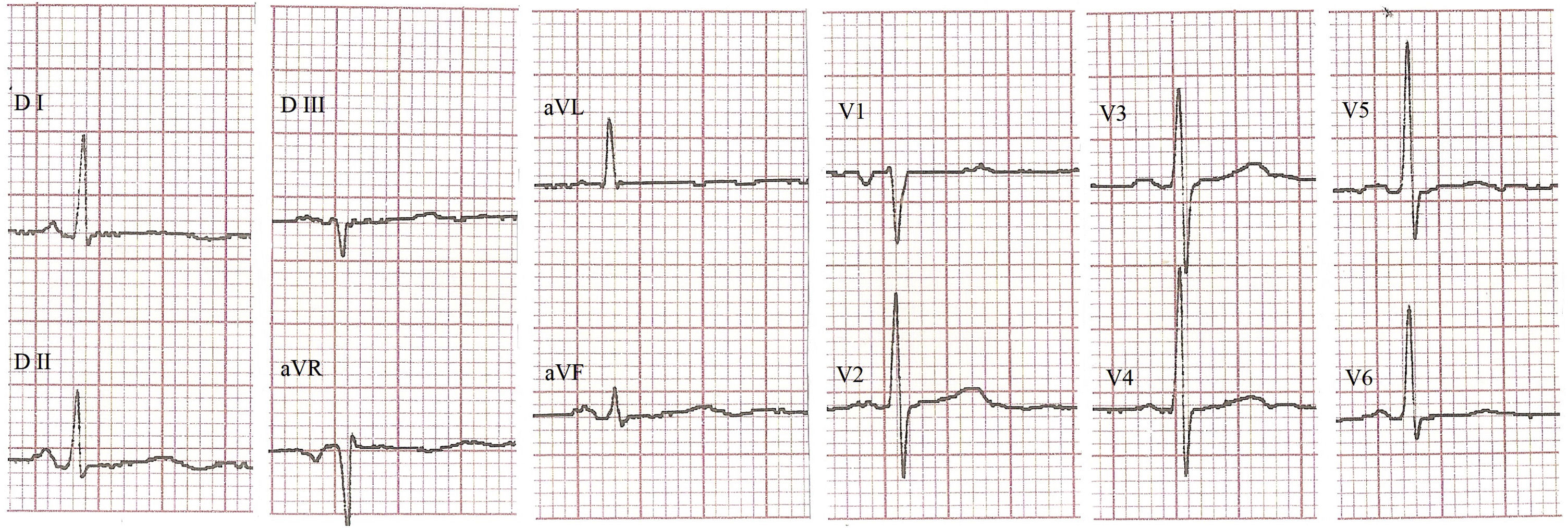
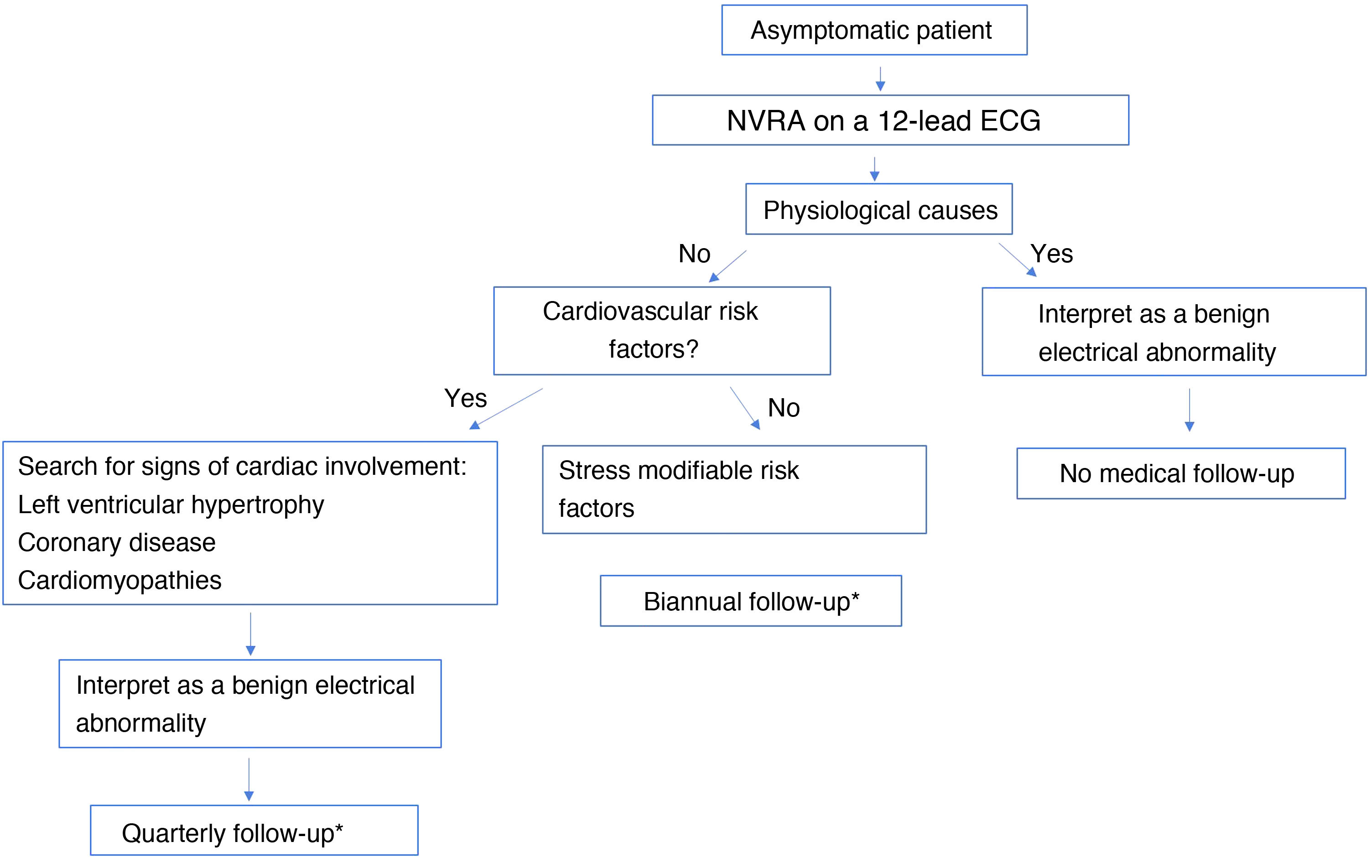
The term nonspecific ventricular repolarization abnormalities refers to a set of minor alterations of the ST segment and/or the T wave. For a long time, they have been of little clinical interest as they do not translate into specific diagnoses. It has even been asserted that they constitute benign electrocardiographic findings. Their presence has been reported in various cardiovascular and non-cardiovascular diseases. However, it is frequently identified in apparently healthy asymptomatic people. A growing number of studies demonstrate their importance as predictors of cardiovascular morbidity and mortality, expanding their spectrum towards cardiovascular prevention. In light of the body of scientific evidence, it is imperative that the traditional view of nonspecific ventricular repolarization abnormalities changes.
El término trastornos inespecíficos de la repolarización ventricular se refiere a un conjunto de alteraciones menores del segmento ST y/o la onda T. Durante mucho tiempo han sido de escaso interés clínico al no traducir diagnósticos específicos. De forma extrema, se ha aseverado que constituyen hallazgos electrocardiográficos benignos. Su presencia se ha reportado en diversos estados patológicos cardiovasculares y no cardiovasculares. Sin embargo, con frecuencia se identifica en personas asintomáticas aparentemente sanas. Un creciente número de estudios demuestran su importancia como predictores de morbimortalidad cardiovascular, expandiendo su espectro hacia la prevención cardiovascular. A la luz de las evidencias científicas acumuladas se impone un cambio en la visión tradicional que se ha tenido con los trastornos inespecíficos de la repolarización ventricular.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<