Although the reasons are unknown, the prevalence of arterial hypertension and atherosclerotic cardiovascular events in the adult population with Down syndrome (SD) is anecdotal. To better understand this finding, we evaluated the haemodynamic characteristics of a cohort of adults with SD.
MethodsWe conducted a cross-sectional study of adults with SD recruited consecutively from the outpatient clinics of an internal medicine department between June and November 2018. We collected demographic, clinical and laboratory variables and employed a thoracic bioimpedance device (HOTMAN® System) for the haemodynamic measures. Outpatient blood pressure monitoring (OBPM) was conducted on a subgroup of participants.
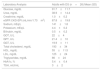
ResultsTwenty-six participants (mean age, 45±11 years) participated in the study (50 % men). The sample’s mean blood pressure (BP) was 109/69±11/9mm Hg, with a mean heart rate of 60±12 bpm. None of the participants had hypertension. The predominant haemodynamic profile consisted of normal dynamism (65 %), normal BP (96 %), hypochronotropism (46 %), normal inotropism (50 %) and hypervolaemia (54 %), with normal peripheral vascular resistance values (58 %). Twelve participants underwent OBPM (46 %). The mean 24-h systolic BP, diastolic BP, mean BP and mean heart rate were 105±11mm Hg, 67±11mm Hg, 80±11mm Hg and 61±6 bpm, respectively.
ConclusionsThe most common haemodynamic profile observed in adults with SD consisted of hypochronotropism and hypervolaemia, with normal values for peripheral vascular resistance and optimal mean BP values. There were no participants with hypertension in our sample.
Si bien se desconocen los motivos, la prevalencia de hipertensión arterial y de eventos cardiovasculares ateroscleróticos en la población adulta con síndrome de Down (SD) es anecdótica. Para entender mejor este hallazgo evaluamos las características hemodinámicas de una cohorte de adultos con SD.
MétodosEstudio transversal en adultos con SD reclutados de modo consecutivo de las consultas externas del servicio de M. Interna entre junio y noviembre 2018. Se recogieron variables demográficas, clínicas y analíticas. Se utilizó un dispositivo de bioimpedancia torácica (HOTMAN® System) para las medidas hemodinámicas. Se realizó una monitorización ambulatoria de presión arterial (MAPA) en un subgrupo de sujetos.
ResultadosVeintiséis sujetos de edad media 45±11 años participaron en el estudio (50% varones). La presión arterial (PA) media en la muestra fue de 109/69±11/9mmHg, con una frecuencia cardiaca media de 60±12 lpm. Ningún sujeto era hipertenso. El perfil hemodinámico predominante consistió en normodinamismo (65%), normotensión (96%), hipocronotropismo (46%), normoinotropismo (50%) ehipervolemia (54%), con valores normales de resistencias vasculares periféricas (58%). Se realizó una MAPA a 12 sujetos (46%). Los valores medios en 24h de PA sistólica fueron 105±11mmHg, PA diastólica 67±11mmHg, PA media 80±11mmHg y frecuencia cardiaca media 61±6 lpm.
ConclusionesEl perfil hemodinámico más frecuentemente observado en adultos con SD consistió en hipocronotropismo e hjpervolemia, con valores normales de resistencias vasculares periféricas y valores medios óptimos de PA. No identificamos ningún sujeto hipertenso en nuestra muestra.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<