Several studies have reported that a higher degree of hemoconcentration in patients admitted for the treatment of acute heart failure (HF) constitutes a favorable prognostic factor in the year following the index episode. The objective of this study was to evaluate whether the highest degree of hemoconcentration at 3 months after admission for HF is also a prognostic factor for mortality and/or readmission in the 12 months after admission.
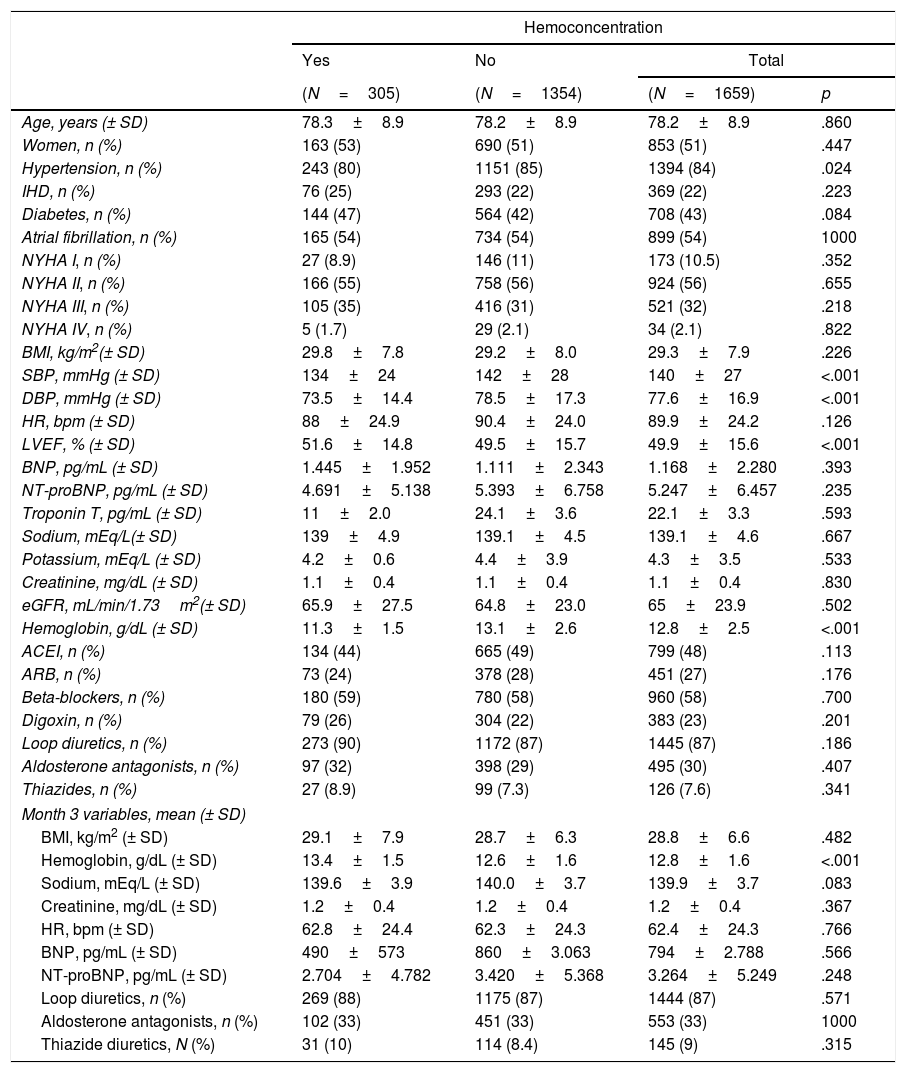
Patients and methodThe hemoconcentration group was the upper quartile of the sample distributed according to hemoglobin increase at month 3 after discharge with respect to hemoglobin at the time of admission for HF in a multicenter prospective cohort of 1659 subjects with HF.
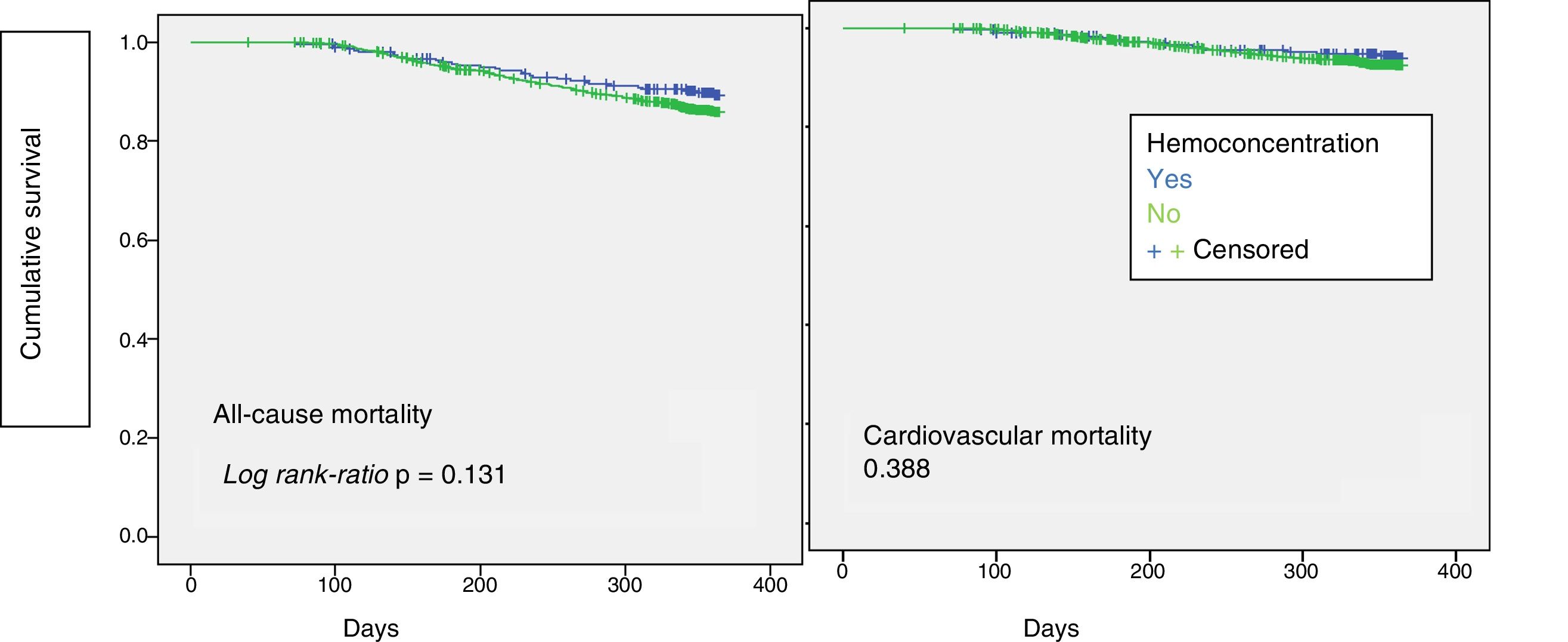
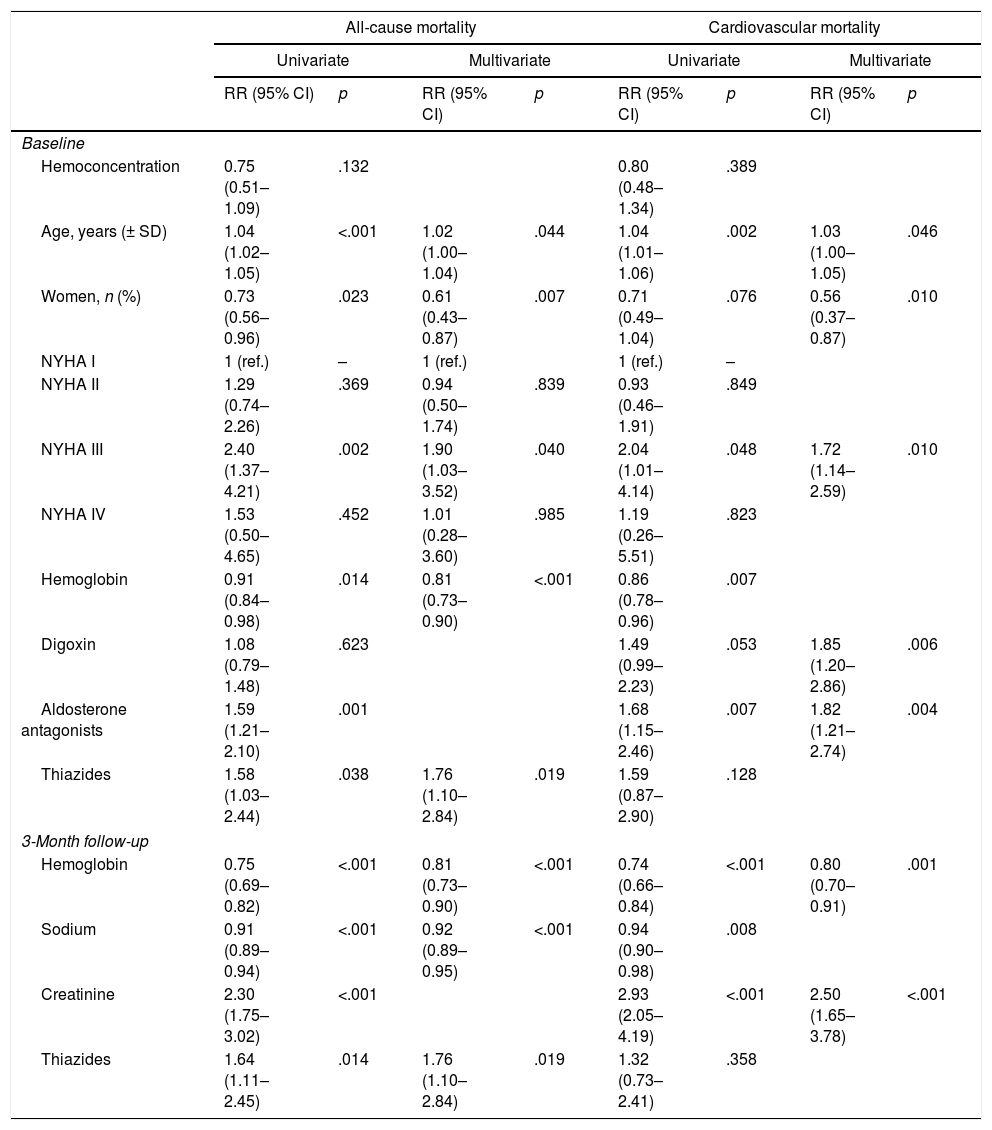
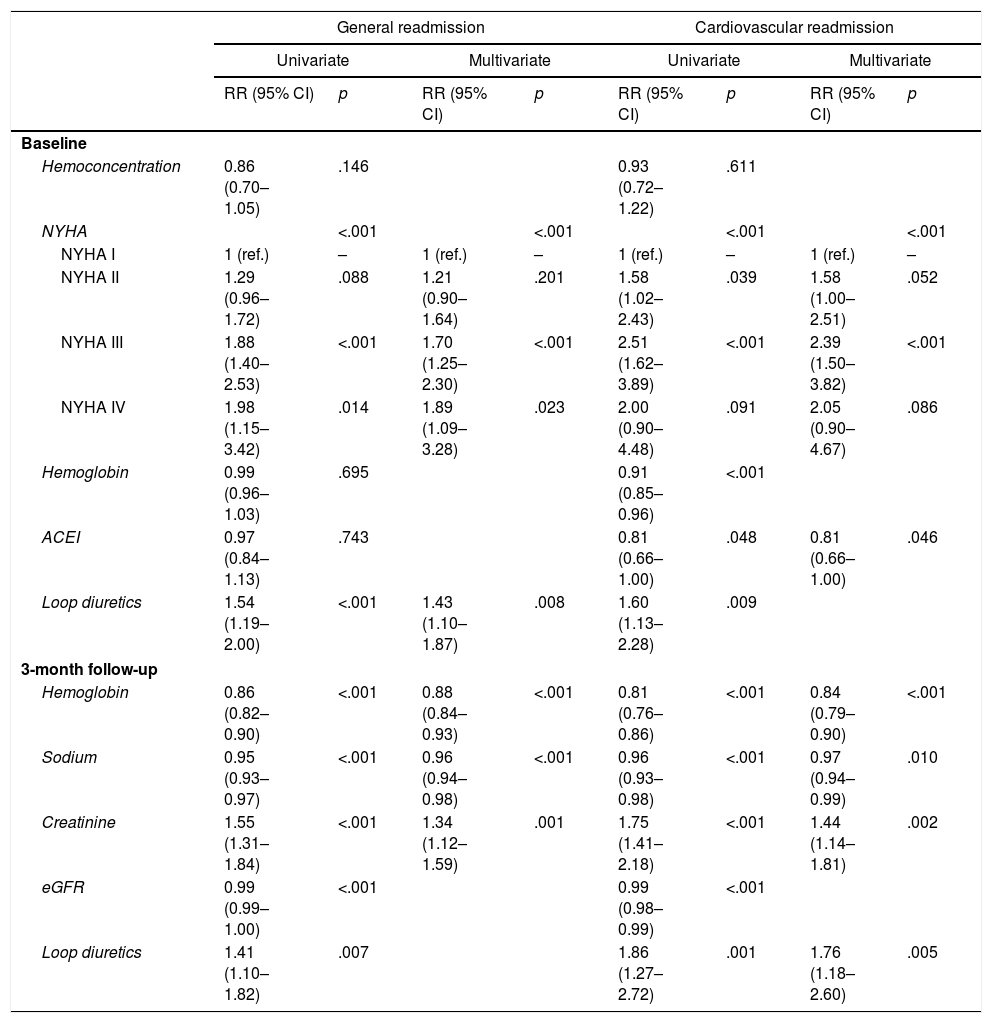
ResultsThe mean follow-up until the first event was 294 days, and a total of 487 deaths and 1125 readmissions were recorded. The hemoconcentration group had a lower risk of mortality or readmission for any cause (RR=0.75, 95% CI: 0.51–1.09 and RR=0.86, 95% CI: 0.70–1.05), although statistical significance was lost after multivariate analysis, while it was retained for other factors with recognized negative impact on the prognosis of patients with HF, such as age and functional class.
ConclusionsThe degree of hemoconcentration at 3 months after admission for HF is not prognostic of readmission or death in the subsequent year.
Diferentes estudios señalan que la consecución de una mayor hemoconcentración en pacientes ingresados por insuficiencia cardiaca (IC) aguda mejora el pronóstico a lo largo del año siguiente al episodio índice. El objetivo de este estudio es evaluar si el grado de hemoconcentración a los 3 meses tras el ingreso por IC también tiene valor pronóstico de reingreso y/o mortalidad en los 12 meses siguientes al ingreso.
Pacientes y métodoCohorte prospectiva multicéntrica de 1.659 pacientes con IC. El grupo hemoconcentración (305 pacientes) se situó en el cuartil superior de la muestra distribuida en función del aumento de la hemoglobina en el mes 3 tras el alta con respecto a la hemoglobina en el ingreso por IC.
ResultadosSeguimiento medio hasta el primer evento fue de 294 días, fallecieron 487 pacientes y reingresaron 1.125. El grupo hemoconcentración mostró un riesgo menor de mortalidad o de reingreso por cualquier causa (RR=0,75; IC 95%: 0,51-1,09 y RR=0,86; IC 95%: 0,70-1,05), si bien la significación estadística se perdió tras el análisis multivariado. Sin embargo, esta significación se mantuvo para otros factores con reconocido efecto negativo sobre el pronóstico en pacientes con IC, como son la edad y la clase funcional.
ConclusionesEl grado de hemoconcentración a los 3 meses tras el ingreso por IC no tiene valor pronóstico de reingreso o muerte en el año siguiente.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<