This work aims to identify and validate a risk scale for admission to intensive care units (ICU) in hospitalized patients with coronavirus disease 2019 (COVID-19).
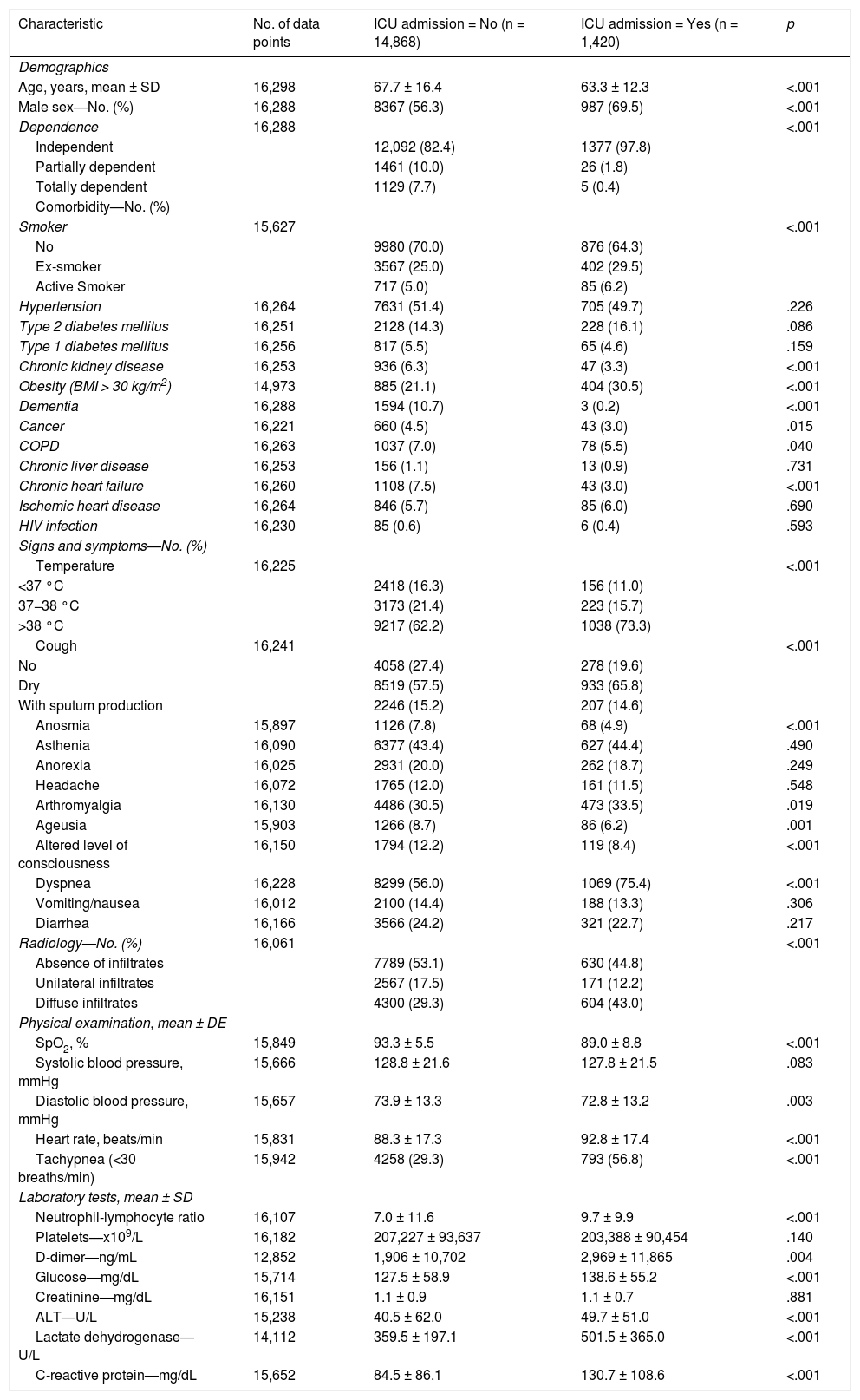
MethodsWe created a derivation rule and a validation rule for ICU admission using data from a national registry of a cohort of patients with confirmed SARS-CoV-2 infection who were admitted between March and August 2020 (N = 16,298). We analyzed the available demographic, clinical, radiological, and laboratory variables recorded at hospital admission. We evaluated the performance of the risk score by estimating the area under the receiver operating characteristic curve (AUROC). Using the β coefficients of the regression model, we developed a score (0–100 points) associated with ICU admission.
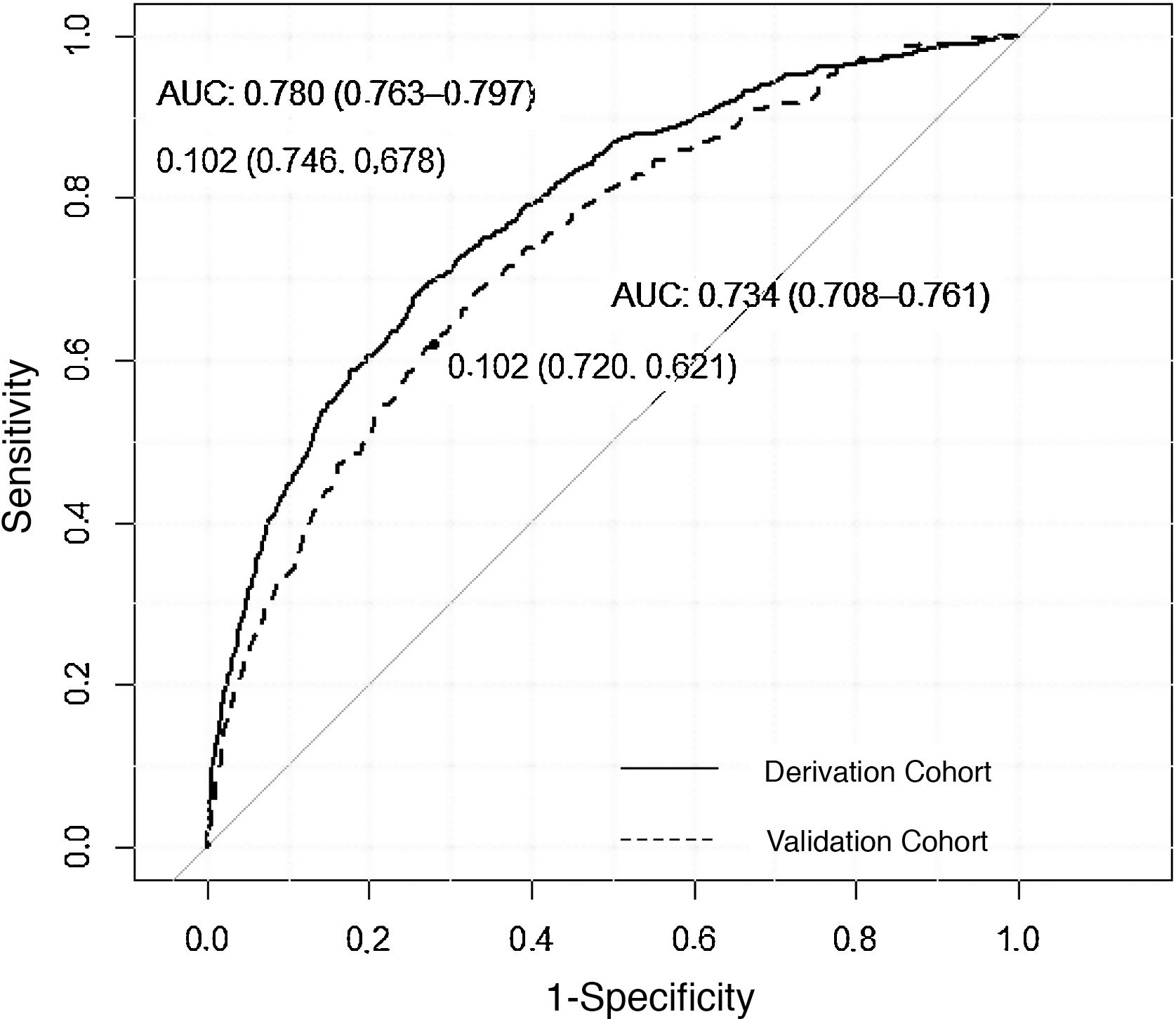
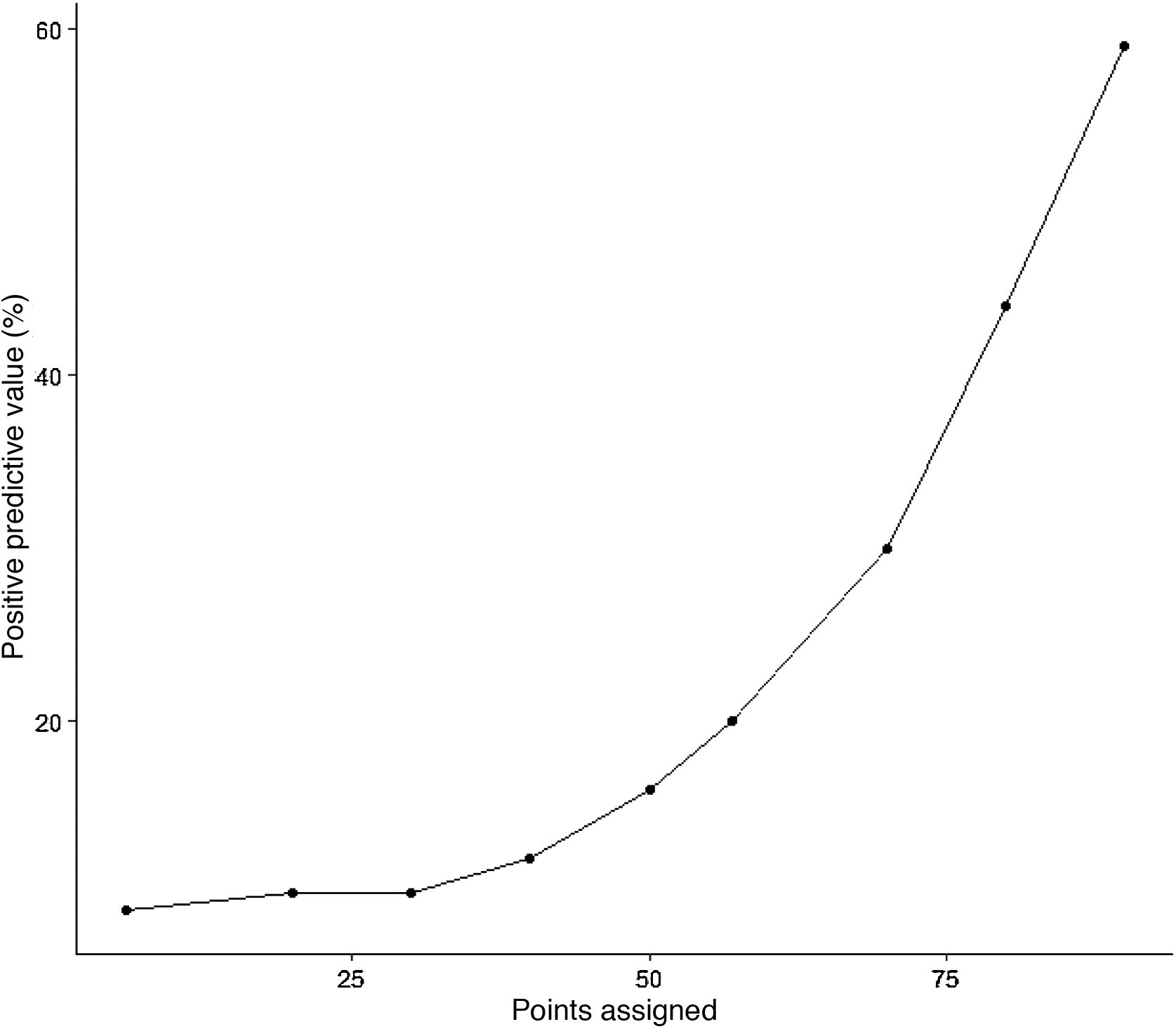
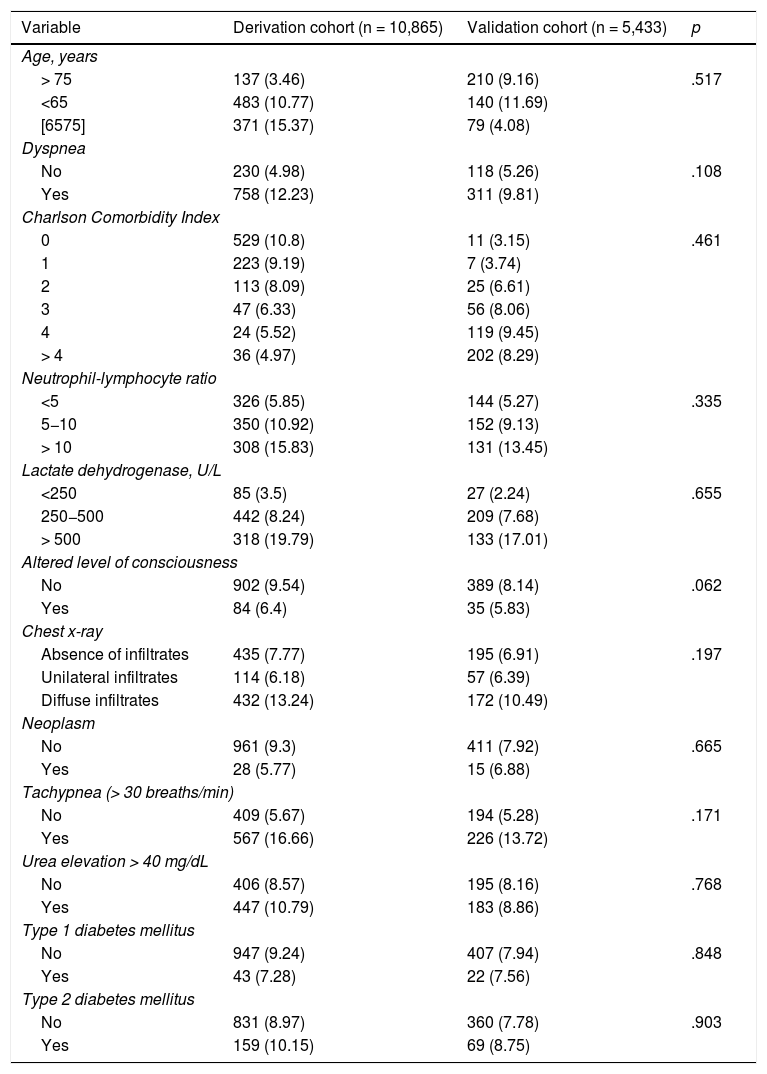
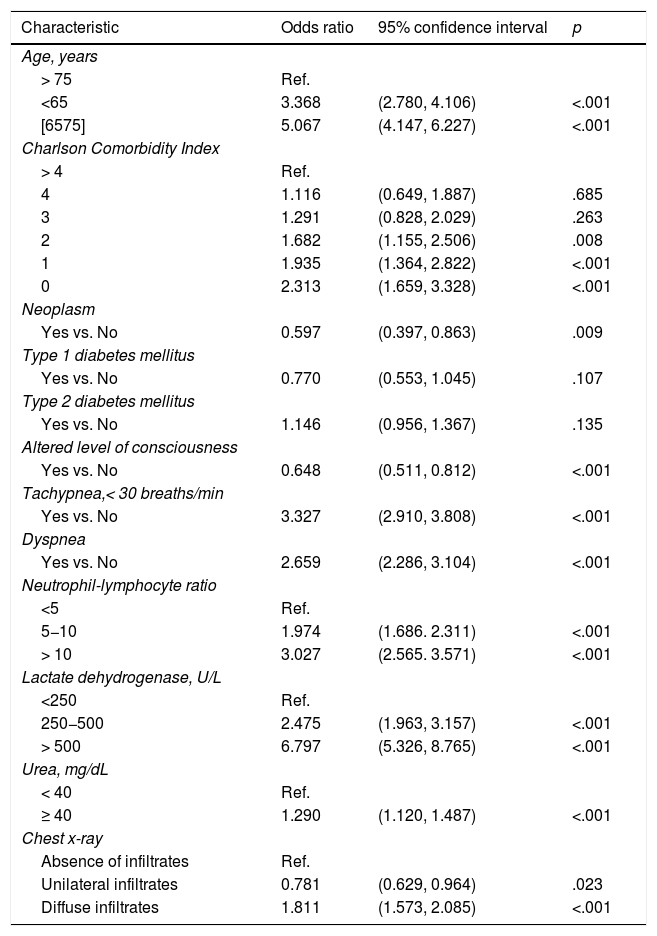
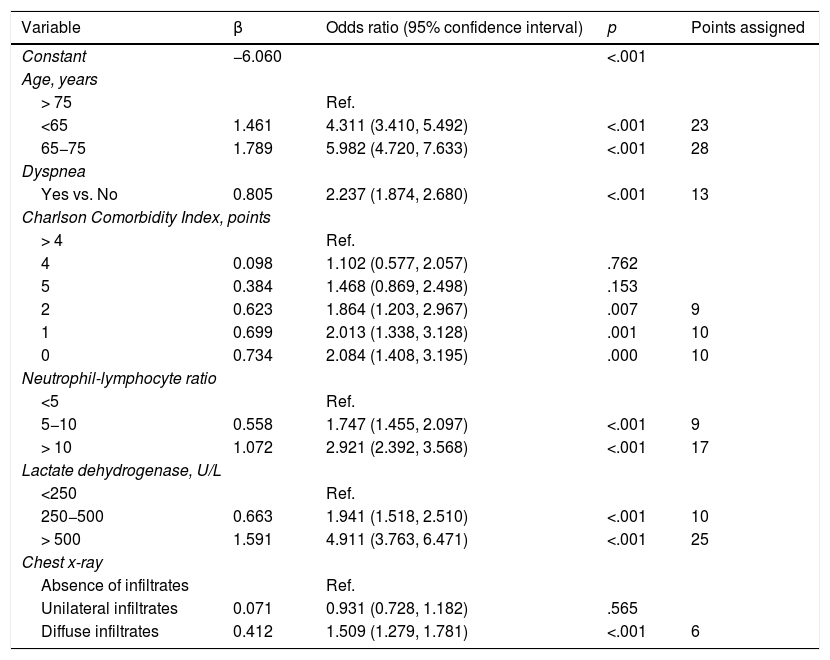
ResultsThe mean age of the patients was 67 years; 57% were men. A total of 1420 (8.7%) patients were admitted to the ICU. The variables independently associated with ICU admission were age, dyspnea, Charlson Comorbidity Index score, neutrophil-to-lymphocyte ratio, lactate dehydrogenase levels, and presence of diffuse infiltrates on a chest X-ray. The model showed an AUROC of 0.780 (CI: 0.763−0.797) in the derivation cohort and an AUROC of 0.734 (CI: 0.708−0.761) in the validation cohort. A score of greater than 75 points was associated with a more than 30% probability of ICU admission while a score of less than 50 points reduced the likelihood of ICU admission to 15%.
ConclusionA simple prediction score was a useful tool for forecasting the probability of ICU admission with a high degree of precision.
Identificar y validar una escala de riesgo de ingreso en las unidades de cuidados intensivos (UCI) en pacientes hospitalizados con enfermedad por coronavirus 2019 (COVID-19).
MétodosRealizamos una regla de derivación y otra de validación para ingreso en UCI utilizando los datos de un registro nacional de cohortes de pacientes con infección confirmada por SARS-CoV-2 ingresados entre marzo y agosto del año 2020 (N = 16.298). Analizamos variables demográficas, clínicas, radiológicas y de laboratorio disponibles en el ingreso hospitalario. Evaluamos el rendimiento de la escala de riesgo mediante estimación del área bajo la curva de característica operativa del receptor (AROC). Utilizamos los coeficientes β del modelo de regresión para elaborar una puntuación (0 a 100 puntos) asociada con ingreso en UCI.
ResultadosLa edad media de los pacientes fue 67 años; 57% varones. Un total de 1.420 (8,7%) pacientes ingresaron en la UCI. Las variables independientes asociadas con el ingreso en UCI fueron: edad, disnea, índice de comorbilidad de Charlson, cociente neutrófilos-linfocitos, lactato deshidrogenasa e infiltrados difusos en la radiografia de tórax. El modelo mostró un AROC de 0,780 (IC: 0,763−0,797) en la cohorte de derivación y un AROC de 0,734 (IC: 0,708−0,761) en la cohorte de validación. Una puntuación > 75 se asoció con una probabilidad de ingreso en UCI superior a un 30%, mientras que una puntuación < 50 redujo la probabilidad de ingreso en UCI al 15%.
ConclusiónUna puntuación de predicción simple proporcionó una herramienta útil para predecir la probabilidad de ingreso en la UCI con un alto grado de precisión.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<