There are few studies on patients with heart failure (HF) hospitalized for COVID-19. Our aim is to describe the clinical characteristics of patients with HF hospitalized for COVID-19 and identify risk factors for in-hospital mortality upon admission.
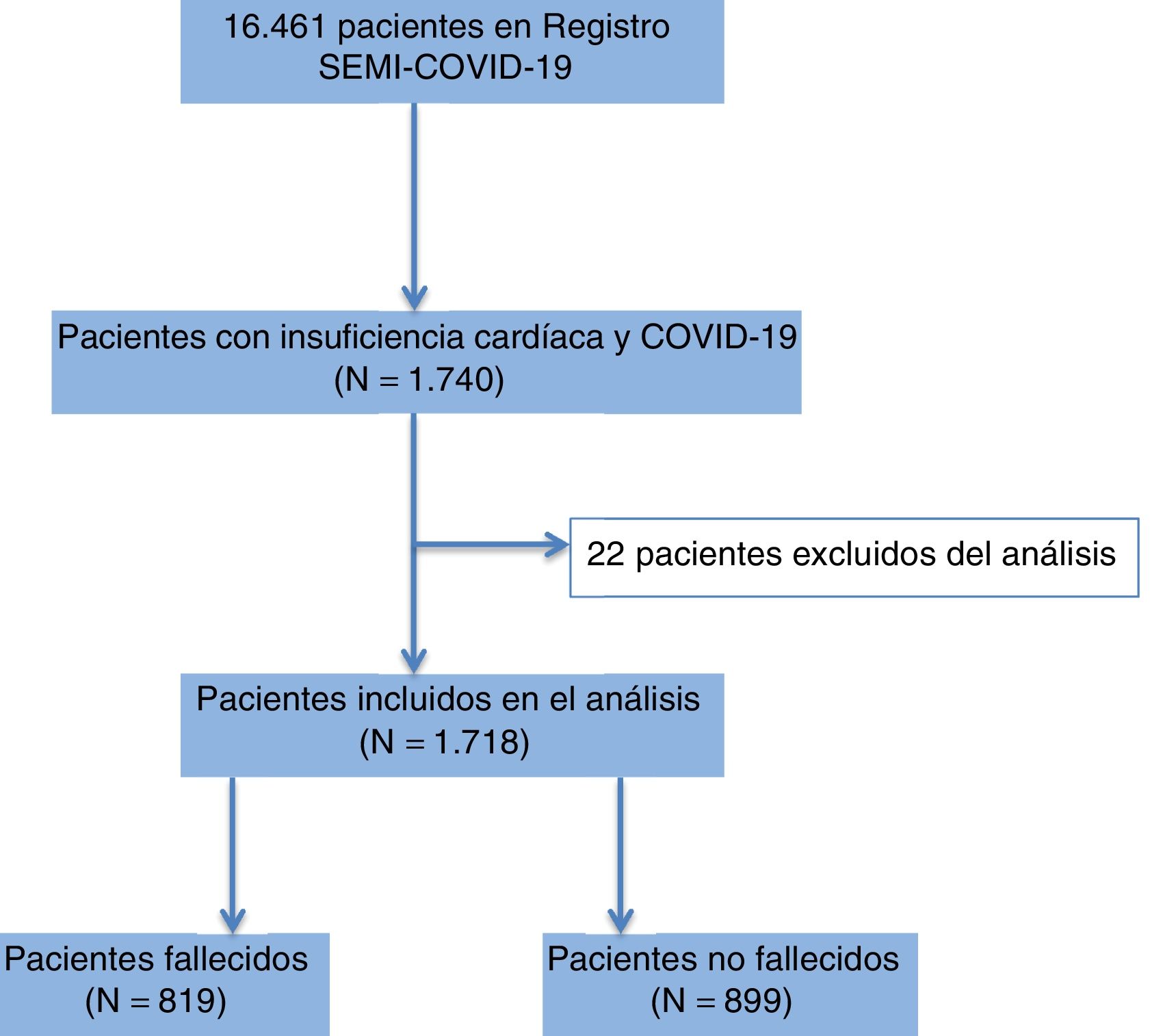
MethodsWe conducted a retrospective, multicenter study in patients with HF hospitalized for COVID-19 in 150 Spanish hospitals (SEMI-COVID-19 Registry). A multivariate logistic regression analysis was performed to identify admission factors associated with in-hospital mortality.
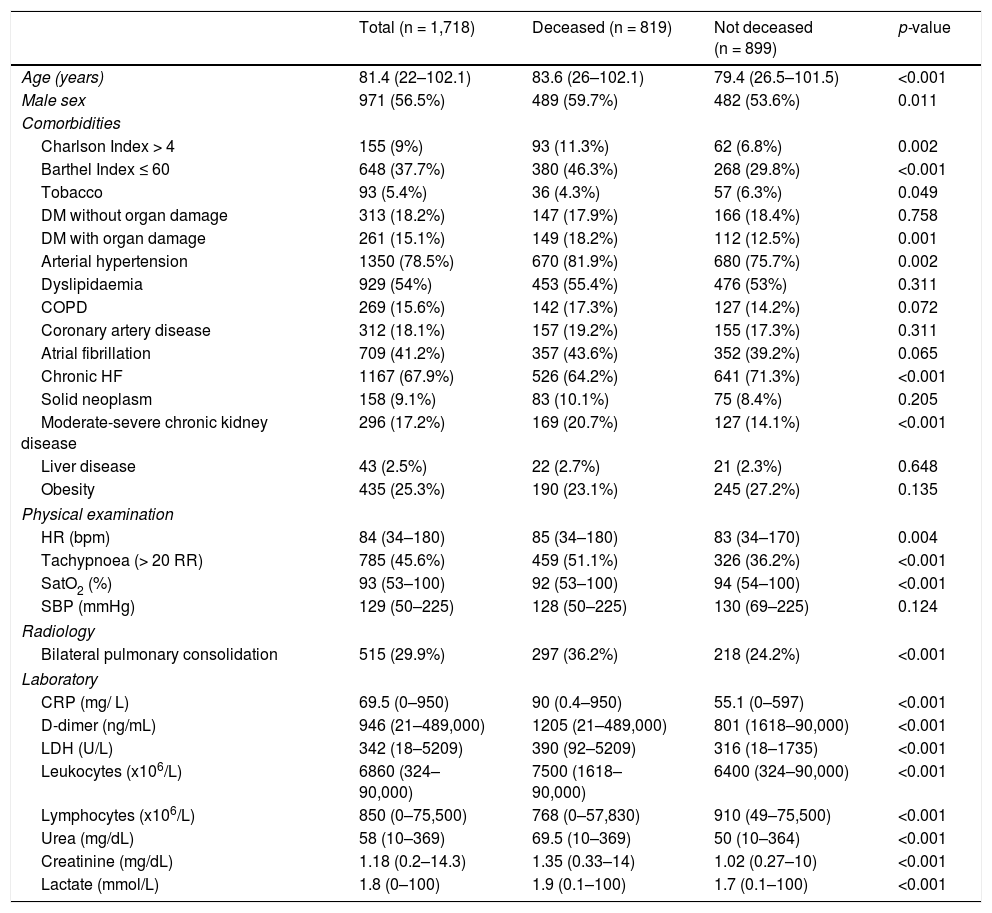
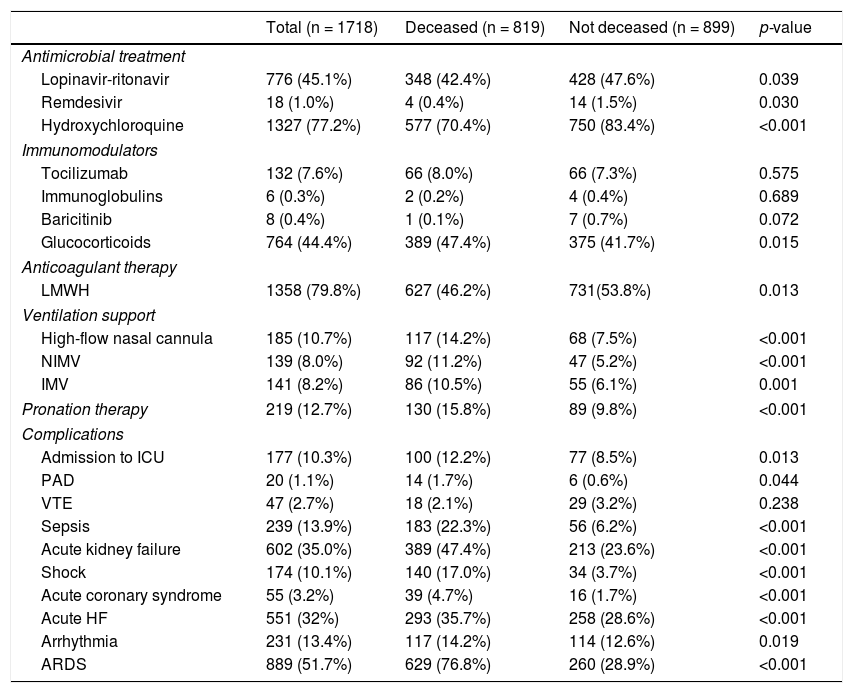
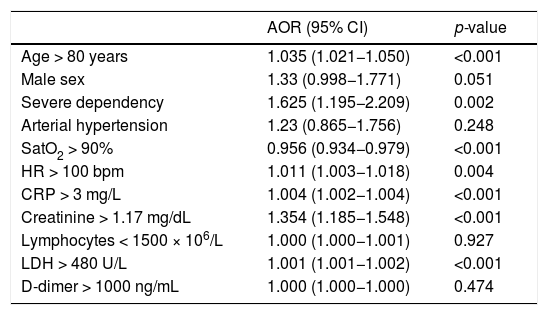
ResultsA total of 1718 patients were analyzed (56.5% men; median age 81.4 years). The overall case fatality rate was 47.6% (n = 819). The independent risk factors at admission for in-hospital mortality were: age (adjusted odds ratio [AOR]: 1.03; 95% confidence interval [95%CI]: 1.02–1.05; p < 0.001); severe dependence (AOR: 1.62; 95%CI: 1.19–2.20; p = 0.002); tachycardia (AOR: 1.01; 95%CI: 1.00–1.01; p = 0.004); and high C-reactive protein (AOR: 1.004; 95%CI:1.002−1.004; p < 0.001), LDH (AOR: 1.001; 95%CI: 1.001−1.002; p < 0.001), and serum creatinine levels (AOR: 1.35; 95%CI: 1.18−1.54; p < 0.001).
ConclusionsPatients with HF hospitalized for COVID-19 have a high in-hospital mortality rate. Some simple clinical and laboratory tests can help to identify patients with a worse prognosis.
Existen pocos estudios sobre pacientes con insuficiencia cardíaca (IC) ingresados por COVID-19. Nuestro objetivo es describir las características clínicas de los pacientes con IC ingresados por COVID-19 e identificar los factores de riesgo al ingreso de mortalidad intrahospitalaria.
Material y métodosEstudio retrospectivo y multicéntrico de pacientes con IC ingresados por COVID-19 en 150 hospitales españoles (Registro SEMI-COVID-19). Se realizó un análisis de regresión logística para identificar los factores de riesgo al ingreso asociados a la mortalidad.
ResultadosSe analizaron 1.718 pacientes (56,5% varones; edad mediana 81,4 años). La tasa de mortalidad global fue del 47,6% (n = 819). Los factores de riesgo independientes al ingreso para mortalidad fueron: la edad (odds ratio ajustado [ORA]: 1,03; intervalo de confianza 95% [IC95%]: 1,02–1,05; p < 0,001), la dependencia severa (ORA: 1,62; IC95%: 1,19–2,20; p = 0,002), la taquicardia (ORA: 1,01; IC95%: 1,00–1,01; p = 0,004), la proteína C reactiva (ORA: 1,004; IC95%:1,002–1,004; p < 0,001), la LDH (ORA: 1,001; IC95%: 1,001–1,002; p < 0,001) y la creatinina sérica (ORA: 1,35; IC95%: 1,18–1,54; p < 0,001).
ConclusionesLos pacientes con IC hospitalizados por COVID-19 tienen una alta mortalidad intrahospitalaria. Existen factores clínico-analíticos simples que pueden ayudar a identificar a los pacientes con peor pronóstico.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.
Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<