To understand the risk factors and long-term impact and results of aortic valve surgery in patients over age 80.
Patients and methodsWe consecutively evaluated 255 octogenarians who were operated on between 2000 and 2013 and referred for aortic valve disease (isolated or combined with coronary artery disease), which, even when associated with other diseases, was the primary cause of the patient's functional limitation.
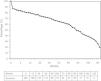
ResultsThe mortality rate decreased from 14.08% (2000–2004) to 7.7% (isolated valve surgery, 4.4%; with coronary bypass, 3.3%) (2010–2013). The independent risk factors associated with mortality were urgent surgery, combined procedures, peripheral vascular disease, a postsurgery hematocrit level <24% and the need for transfusion. More than 50% of the patients experienced a postoperative complication. Blood product transfusions were associated with renal and respiratory failure, and preoperative anemia was associated with an increased rate of myocardial infarction and stroke. Survival at 1, 3, 5 and 10 years was 79.5, 74.3, 63.6 and 30.5%, respectively, with 91.5% of the patients in NYHA functional class I–II. Long-term survival was lower for cases of preoperative left ventricular dysfunction. The EuroSCORE I logistics score was not useful for our population as a predictor of mortality or of medium to long-term survival.
ConclusionsThe morbidity and mortality of aortic valve surgery for patients over age 80 has decreased in recent years, although it remains higher when valve surgery is combined with coronary surgery. The presence of preoperative left ventricular dysfunction decreases long-term survival.
Conocer los factores de riesgo, resultados e impacto a largo plazo de la cirugía valvular aórtica en pacientes con más de 80 años.
Pacientes y métodosEvaluamos 255 octogenarios consecutivos, intervenidos entre 2000 y 2013, y remitidos por valvulopatía aórtica (aislada o combinada con enfermedad coronaria) que, aun asociada a otras patologías, era la causa principal de limitación funcional del paciente.
ResultadosLa mortalidad se redujo del 14,08% (periodo 2000–2004) al 7,7% (cirugía valvular aislada, 4,4% y con bypass coronario, 3,3%) (periodo 2010–2013). La cirugía urgente, los procedimientos combinados, la enfermedad vascular periférica, un hematocrito postquirúrgico <24% y la necesidad de transfusión, fueron factores de riesgo independientes asociados a la mortalidad. Más del 50% de los pacientes presentó alguna complicación postoperatoria. La transfusión de hemoderivados se asoció a insuficiencia renal y respiratoria, y la anemia preoperatoria a mayor frecuencia de infarto de miocardio e ictus. La supervivencia a 1, 3, 5 y 10 años fue del 79,5; 74,3; 63,6 y 30,5%, respectivamente, con un 91,5% de los pacientes en clase funcional NYHA I-II. La supervivencia a largo plazo se redujo en caso de disfunción ventricular izquierda preoperatoria. La puntuación EuroSCORE I logística no resultó útil en nuestra población como predictor de mortalidad ni de supervivencia a medio-largo plazo.
ConclusionesLa morbimortalidad de la cirugía valvular aórtica en los pacientes con más de 80 años ha descendido en los últimos años, aunque sigue siendo superior cuando la cirugía valvular se asocia a cirugía coronaria. La presencia de disfunción ventricular izquierda preoperatoria disminuye la supervivencia a largo plazo.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<