Ultrasonography has been shown to be a useful tool for diagnosing pneumothorax in the hands of experts. After performing bronchopleural procedures, the recommendation is to perform chest radiography to rule out complications. Our objective was to determine the validity of lung ultrasound, conducted by pulmonologists without experience in this procedure, to tule out pneumothorax after invasive procedures.
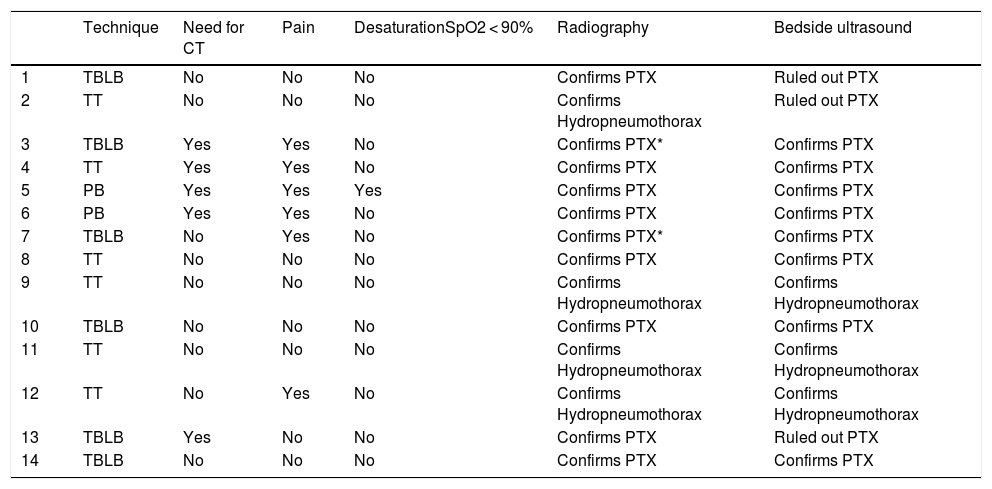
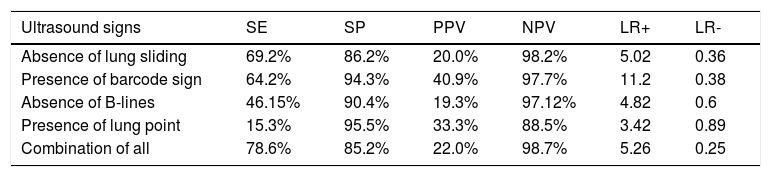
Material and MethodsOur prospective observational study consecutively included patients who underwent transbronchial lung biopsy (TBLB), therapeutic thoracentesis (TT) and/or transparietal pleural biopsies (PB) for whom subsequent chest radiography to rule out complications was indicated. In all cases, the same pulmonologist who performed the technique performed an ultrasound immediately after the procedure. A diagnosis of pneumothorax was considered in the presence of a lung point or the combination of the following signs: absence of pleural sliding, absence of B-lines and presence of the “barcode” sign.
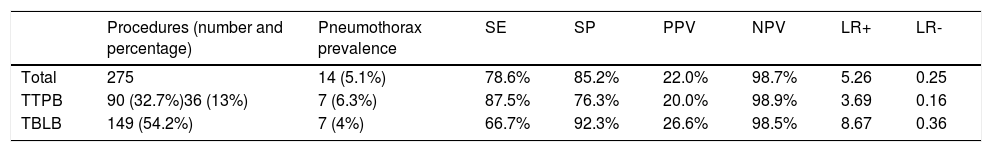
ResultsWe included 275 procedures (149 TBLBs, 36 BPs, 90 TTs), which resulted in 14 (5.1%) iatrogenic pneumothoraxes. Ultrasonography presented a sensitivity of 78.5%, a specificity of 85% and positive and negative predictive value of 22% and 98.6%, respectively. Ultrasonography did not help detect the presence of 3 pneumothoraxes, one of which required chest drainage, but adequately diagnosed 2 pneumothoraxes that were not identified in the initial radiography.
ConclusionsLung ultrasound performed by pulmonologists at the start of their training helps rule out pneumothorax with a negative predictive value of 98.6%, thereby avoiding unnecessary radiographic control studies in a considerable number of cases.
La ecografía ha demostrado ser una herramienta útil para el diagnóstico del neumotórax en manos expertas. Tras los procedimientos broncopleurales se recomienda realizar una radiografía de tórax para descartar complicaciones. Nuestro objetivo ha sido determinar la validez de la ecografía torácica para descartar neumotórax tras procedimientos invasivos, realizada por neumólogos sin experiencia en este procedimiento.
Material y métodosEstudio observacional prospectivo que incluyó pacientes consecutivos sometidos a biopsia transbronquial (BTB), toracocentesis evacuadora (TE) y/o biopsias pleurales transparietales (BPT) a los que se les indicó radiografía de tórax posterior para descartar complicaciones. En todos los casos el mismo neumólogo que hizo la técnica, realizó una ecografía inmediatamente después del procedimiento. Se consideró diagnóstica de neumotórax la presencia de punto pulmonar o la combinación de los signos: ausencia de deslizamiento pleural, ausencia de líneas B y presencia del signo de «código de barras».
ResultadosSe incluyeron 275 procedimientos (149 BTB, 36 BPT, 90 TE) entre los que se produjeron 14 (5,1%) neumotórax iatrogénicos. La ecografía presentó una sensibilidad de 78,5%, una especificidad de 85%, y un valor predictivo positivo y negativo de 22% y 98,6% respectivamente. La ecografía no permitió detectar la presencia de 3 neumotórax, precisando uno de ellos drenaje torácico y diagnosticó adecuadamente dos neumotórax que no se detectaban en la radiografía inicial.
ConclusionesLa ecografía torácica realizada por neumólogos que inician su curva de aprendizaje permite descartar neumotórax con un VPN del 98,6%, evitando realizar en un número considerable de casos estudios radiográficos de control innecesarios.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<