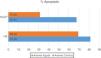
Increasing haemoglobin and haematocrit levels with blood transfusions has been the gold standard for treating severe anaemia; however, the indication for transfusing concentrated red blood cells is based merely on a few laboratory markers, such as haemoglobin and haematocrit levels, rather than based on the symptoms according to clinical practice guidelines, the implementation of legal regulations and the consensus achieved by the hospitals’ transfusion committees. The aim of this multicentre study was to reassess the suitability of the indication for transfusing concentrated red blood cells and the volumes transfused in emergency departments. We established an observational, multicentre, cross-sectional design with 2 participating centres: the La Paz University Hospital and the Hospital of Salamanca. In total, we obtained data from 381 patients, 220 (57.74%) of whom were men with an average age of 71.4±14.0 years and 161 (42.26%) of whom were women with an average age of 75.3±15.3 years (P<0.001). The most prevalent underlying diseases in the patients who underwent transfusions were heart disease, which included haemorrhaging due to antiplatelet or anticoagulant therapy (57.7%), haematooncologic (15.3%) diseases and neurological disease. Only 54.9% (209/381) of the prescriptions for transfusion were considered appropriate, with significant differences according to the indication.
La elevación del nivel de hemoglobina y de hematocrito con transfusiones sanguíneas ha sido el estándar de oro para el tratamiento de la anemia grave. Sin embargo, la indicación para la transfusión de concentrado de hematíes se basa meramente en unos marcadores analíticos, como el nivel de hemoglobina o hematocritos, en lugar de basarse en la clínica (según las guías de práctica clínica), en la implementación de regulaciones legales o en los consensos alcanzados por los comités de transfusión de los hospitales. El objetivo de este estudio multicéntrico es reevaluar la idoneidad de la indicación de transfusión de concentrado de hematíes y los volúmenes transfundidos en los servicios de urgencias. Se plantea un diseño observacional multicéntrico y transversal en 2 centros participantes: el Hospital Universitario de La Paz y el Hospital de Salamanca. En total se obtuvieron datos de 381 pacientes; 220 eran hombres (57,74%), con una edad promedio de 71,4±14,0 años y 161 eran mujeres (42,26% con una edad promedio de 75,3±15,3 años p<0,001. Las enfermedades subyacentes más prevalentes en los pacientes que recibieron transfusión fueron las cardiológicas, que incluyeron hemorragia debido a la terapia antiagregante plaquetaria o anticoagulante 57.7%), las hematooncológicas (15.3%) y las neurológicas. Solo el 54.9% (209/381) de las prescripciones de transfusión se consideraron apropiadas, con diferencias significativas observadas según la indicación.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<