COVID-19 is responsible for high mortality in elderly patients.1–3 In turn, elderly individuals may experience increased dependence in daily living activities and frailty as a result of diminished physiological reserve, placing them at risk of adverse outcomes (functional limitation and death).4,5
Different studies have investigated frailty in COVID-19 patients as a mortality risk factor.2,6 A number of studies have also evidenced that dependence in daily living activities is likewise associated to increased mortality in older patients.7 However, this issue has not been studied so much in depth in the context of infection due to the Omicron variant of COVID-19, which produced less mortality but greater disease transmission.2 Similarly, few studies are available on changes in dependence and frailty among patients with COVID-19.8,9
Thus, the study we have carried out aims to analyze dependence and frailty as a predictor of mortality and to describe the changes in dependence and frailty in elderly people with COVID-19 who required admission during the pandemic wave due to the Omicron variant of the virus.
An analysis was made of the patients over 65 years of age admitted to the Department of Internal Medicine from 7 January 2022 to 28 February 2022. Dependence was analyzed based on the Barthel index,4 and frailty was assessed using the Frail scale described by Fried et al.10 The risk of falls was studied using the Downton scale. The Barthel index and the Frail scale were applied 15 days before admission (baseline), at the time of admission, at hospital discharge, and 15 days after hospital discharge (via a telephone call).
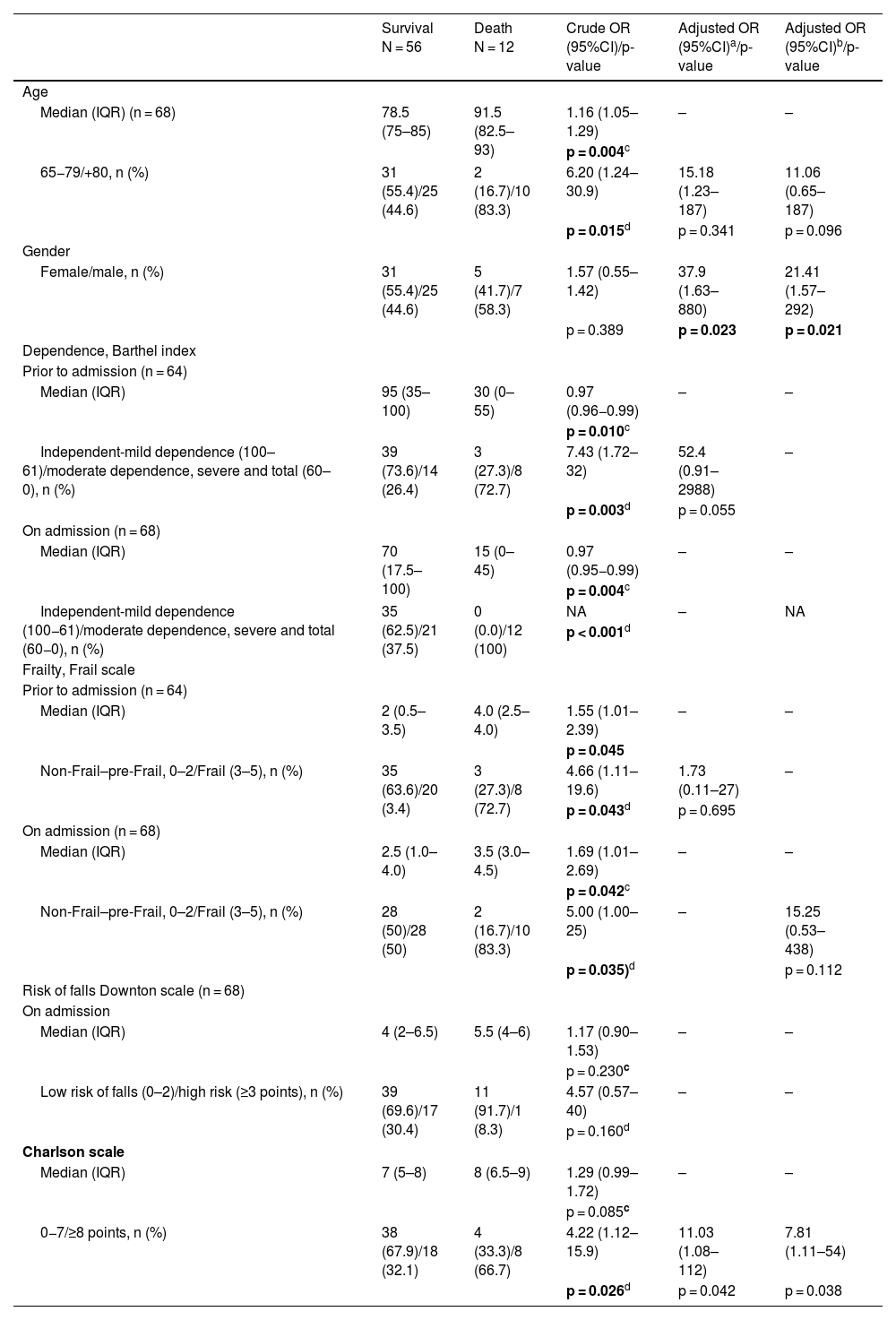
During the study period, 68 patients over 65 years of age with COVID-19 were admitted, and 12 patients died during admission or within 15 days after discharge (17.6%). Those who died had a significantly greater mean age (91.5 vs 78.5 years; p = 0.002), a lower Barthel score before admission and at the time of admission (median: 30 and 15 vs 95 and 70; p < 0.01), and a higher Frail score before admission and at the time of admission (median: 4.0 and 3.5 vs 2 and 2.5; p = 0.050). The Downton scale and gender were not related to mortality. The age-adjusted Charlson comorbidity index was higher in those who died (median: 8 vs 7; p = 0.085) (Table 1).
Association between age, gender, level of dependence, frailty, risk of falls and comorbidity in patients over 65 years of age with COVID-19 and an unfavorable course, and changes observed during admission and up to 15 days after discharge.
| Survival N = 56 | Death N = 12 | Crude OR (95%CI)/p-value | Adjusted OR (95%CI)a/p-value | Adjusted OR (95%CI)b/p-value | |
|---|---|---|---|---|---|
| Age | |||||
| Median (IQR) (n = 68) | 78.5 (75–85) | 91.5 (82.5–93) | 1.16 (1.05–1.29) | – | – |
| p = 0.004c | |||||
| 65−79/+80, n (%) | 31 (55.4)/25 (44.6) | 2 (16.7)/10 (83.3) | 6.20 (1.24–30.9) | 15.18 (1.23–187) | 11.06 (0.65–187) |
| p = 0.015d | p = 0.341 | p = 0.096 | |||
| Gender | |||||
| Female/male, n (%) | 31 (55.4)/25 (44.6) | 5 (41.7)/7 (58.3) | 1.57 (0.55–1.42) | 37.9 (1.63–880) | 21.41 (1.57–292) |
| p = 0.389 | p = 0.023 | p = 0.021 | |||
| Dependence, Barthel index | |||||
| Prior to admission (n = 64) | |||||
| Median (IQR) | 95 (35–100) | 30 (0–55) | 0.97 (0.96−0.99) | – | – |
| p = 0.010c | |||||
| Independent-mild dependence (100–61)/moderate dependence, severe and total (60–0), n (%) | 39 (73.6)/14 (26.4) | 3 (27.3)/8 (72.7) | 7.43 (1.72–32) | 52.4 (0.91–2988) | – |
| p = 0.003d | p = 0.055 | ||||
| On admission (n = 68) | |||||
| Median (IQR) | 70 (17.5–100) | 15 (0–45) | 0.97 (0.95−0.99) | – | – |
| p = 0.004c | |||||
| Independent-mild dependence (100−61)/moderate dependence, severe and total (60−0), n (%) | 35 (62.5)/21 (37.5) | 0 (0.0)/12 (100) | NA | – | NA |
| p < 0.001d | |||||
| Frailty, Frail scale | |||||
| Prior to admission (n = 64) | |||||
| Median (IQR) | 2 (0.5–3.5) | 4.0 (2.5–4.0) | 1.55 (1.01–2.39) | – | – |
| p = 0.045 | |||||
| Non-Frail–pre-Frail, 0–2/Frail (3–5), n (%) | 35 (63.6)/20 (3.4) | 3 (27.3)/8 (72.7) | 4.66 (1.11–19.6) | 1.73 (0.11–27) | – |
| p = 0.043d | p = 0.695 | ||||
| On admission (n = 68) | |||||
| Median (IQR) | 2.5 (1.0–4.0) | 3.5 (3.0–4.5) | 1.69 (1.01–2.69) | – | – |
| p = 0.042c | |||||
| Non-Frail–pre-Frail, 0–2/Frail (3–5), n (%) | 28 (50)/28 (50) | 2 (16.7)/10 (83.3) | 5.00 (1.00–25) | – | 15.25 (0.53–438) |
| p = 0.035)d | p = 0.112 | ||||
| Risk of falls Downton scale (n = 68) | |||||
| On admission | |||||
| Median (IQR) | 4 (2–6.5) | 5.5 (4–6) | 1.17 (0.90–1.53) | – | – |
| p = 0.230c | |||||
| Low risk of falls (0–2)/high risk (≥3 points), n (%) | 39 (69.6)/17 (30.4) | 11 (91.7)/1 (8.3) | 4.57 (0.57–40) | – | – |
| p = 0.160d | |||||
| Charlson scale | |||||
| Median (IQR) | 7 (5–8) | 8 (6.5–9) | 1.29 (0.99–1.72) | – | – |
| p = 0.085c | |||||
| 0−7/≥8 points, n (%) | 38 (67.9)/18 (32.1) | 4 (33.3)/8 (66.7) | 4.22 (1.12–15.9) | 11.03 (1.08–112) | 7.81 (1.11–54) |
| p = 0.026d | p = 0.042 | p = 0.038 | |||
| Evolution of dependence and frailty | |||||
|---|---|---|---|---|---|
| 15 days prior to admission | On admission | At discharge | After 15 days | P-value | |
| Dependence, Barthel index | |||||
| Median (IQR) | 95 (65–100) | 72.5 (20–100) | 85 (10–100) | 82 (25–100) | 0.032e |
| Independent-mild dependence (100−61)/moderate dependence, severe and total (60–0), n (%) | 42 (65.6)/22 (34.4) | 35 (51.5)/33 (48.5) | 33 (52.4)/30 (47.6) | 32 (57.1)/24 (42.9) | 0.080 |
| Frailty, Frail scale | |||||
| Median (IQR) | 2 (0–2) | 2 (1–4) | 2.5 (1–4) | 2 (1–4) | 0.101e |
| Non-Frail–pre-Frail, 0–2/Frail (3–5), n (%) | 38 (57.6)/28 (42.4) | 30 (44.1)/38 (55.9) | 26 (38.2)/36 (52.9) | 431 (45.6)/25 (44.6) | 0.080 |
Bold values signifies values are statistically significant differences.
Taking into account the results of the multivariate analysis involving the Barthel index, Frail scale, Charlson comorbidity index, age and gender, association to mortality was defined by having a very high Charlson comorbidity index (≥8 points), an age of 80 years or older, and the male gender (Table 1).
The mean Barthel index prior to admission (95 points) decreased up until the time of admission (72.5 points). It subsequently did not worsen during admission and even recovered slightly 15 days after discharge (82 points). The Frail score increased prior to admission – with a worsening of frailty – and improved 15 days after discharge.
This study is limited by its single-center design, with a small number of patients. As strengths, however, it analyzes dependence and frailty as risk factors for mortality, and in particular it explores the changes in these parameters seen in patients requiring admission.
This work shows that dependence and frailty 15 days prior to admission and at the time of admission are risk factors for mortality in patients over 65 years of age with severe COVID-19 disease who require admission due to respiratory failure.
In addition, the levels of dependence and frailty increase upon admission versus baseline 15 days before, and recover slightly after 15 days. Such recovery could be due to the fact that the patients who died were not evaluated (n = 12). Thus, these results on the evolution of the Barthel index and Frail scale should be interpreted with caution. COVID-19 probably increases frailty and patient dependence at discharge, and this persists 15 days after discharge.
Lastly, it should be underscored that due to worsening of their functional status, these patients would benefit from the early adoption of functional and psychosocial rehabilitation measures.