Acute heart failure (AHF) is a highly prevalent clinical entity in individuals older than 45 years in Spain. AHF is associated with significant morbidity and mortality and is the leading cause of hospitalisation for individuals older than 65 years in Spain, a quarter of whom die within 1 year of the hospitalisation. In recent years, there has been an upwards trend in hospitalisations for AHF, which increased 76.7% from 2003 to 2013. Readmissions at 30 days for AHF have also increased (from 17.6% to 22.1%), at a relative mean rate of 1.36% per year, with the consequent increase in the use of resources and the economic burden for the healthcare system. The aim of this document (developed by the Heart Failure and Atrial Fibrillation Group of the Spanish Society of Internal Medicine) is to guide specialists on the most important aspects of treatment and follow-up for patients with AHF during hospitalisation and the subsequent follow-up. The main recommendations listed in this document are as follows: 1) At admission, perform a comprehensive assessment, considering the patient’s standard treatment and comorbidities, given that these determine the disease prognosis to a considerable measure. 2) During the first few hours of hospital care, decongestive treatment is a priority, and a staged diuretic therapeutic approach based on the patient’s response is recommended. 3) To manage patients in the stable phase, consider starting and/or adjusting evidence-based drug treatment (e.g., sacubitril/valsartan or angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers, beta blockers and aldosterone antagonists). 4) At hospital discharge, use a checklist to optimise the patient’s management and identify the most efficient options for maintaining continuity of care after discharge.
La insuficiencia cardiaca aguda (ICA) es una entidad clínica con una elevada prevalencia en la población de más de 45 años en España. Está asociada a una importante morbimortalidad, constituyendo la primera causa de hospitalización en mayores de 65 años en nuestro país, de los cuales una cuarta parte fallecen al año del ingreso. En los últimos años se ha observado una tendencia al alza en las hospitalizaciones por ICA, que aumentaron un 76,7% en el período de 2003 a 2013. Los reingresos a los 30 días por ICA también aumentaron (del 17,6 al 22,1%) a un ritmo medio relativo del 1,36% por año, con el consiguiente increment en el uso de recursos y en la carga económica para el sistema sanitario. Este documento, elaborado por el grupo de Insuficiencia Cardiaca y Fibrilación Auricular de la Sociedad Española de Medicina Interna, tiene como objetivo orientar al especialista en los aspectos más importantes del tratamiento y seguimiento de los pacientes con ICA durante el ingreso y el seguimiento posterior. Las principales recomendaciones recogidas son: 1) en el momento del ingreso, realizar una evaluación integral, considerando el tratamiento habitual y comorbilidades del paciente, ya que condicionan en gran medida el pronóstico de la enfermedad; 2) en las primeras horas de atención hospitalaria, el tratamiento descongestivo es prioritario y se recomienda un abordaje terapéutico diurético escalonado en función de la respuesta; 3) en el manejo de la fase estable, considerar el inicio y/o ajustar el tratamiento con fármacos basados en la evidencia, es decir, sacubitrilo/valsartán o IECA/ARA II, betabloqueantes y antialdosterónicos; 4) en el momento del alta hospitalaria, utilizar un checklist para optimizar el manejo del paciente hospitalizado e identificar las opciones más eficientes para mantener la continuidad de cuidados tras el alta.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.
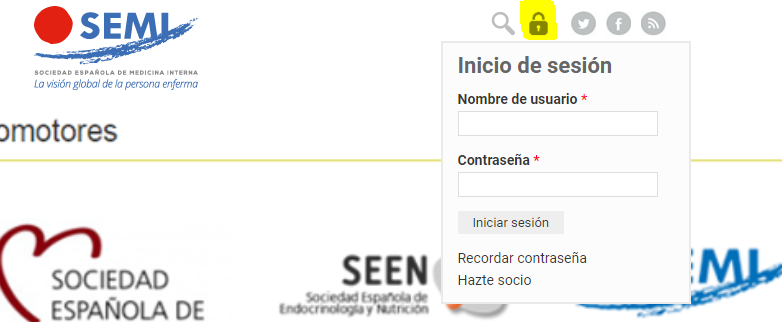
Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<






