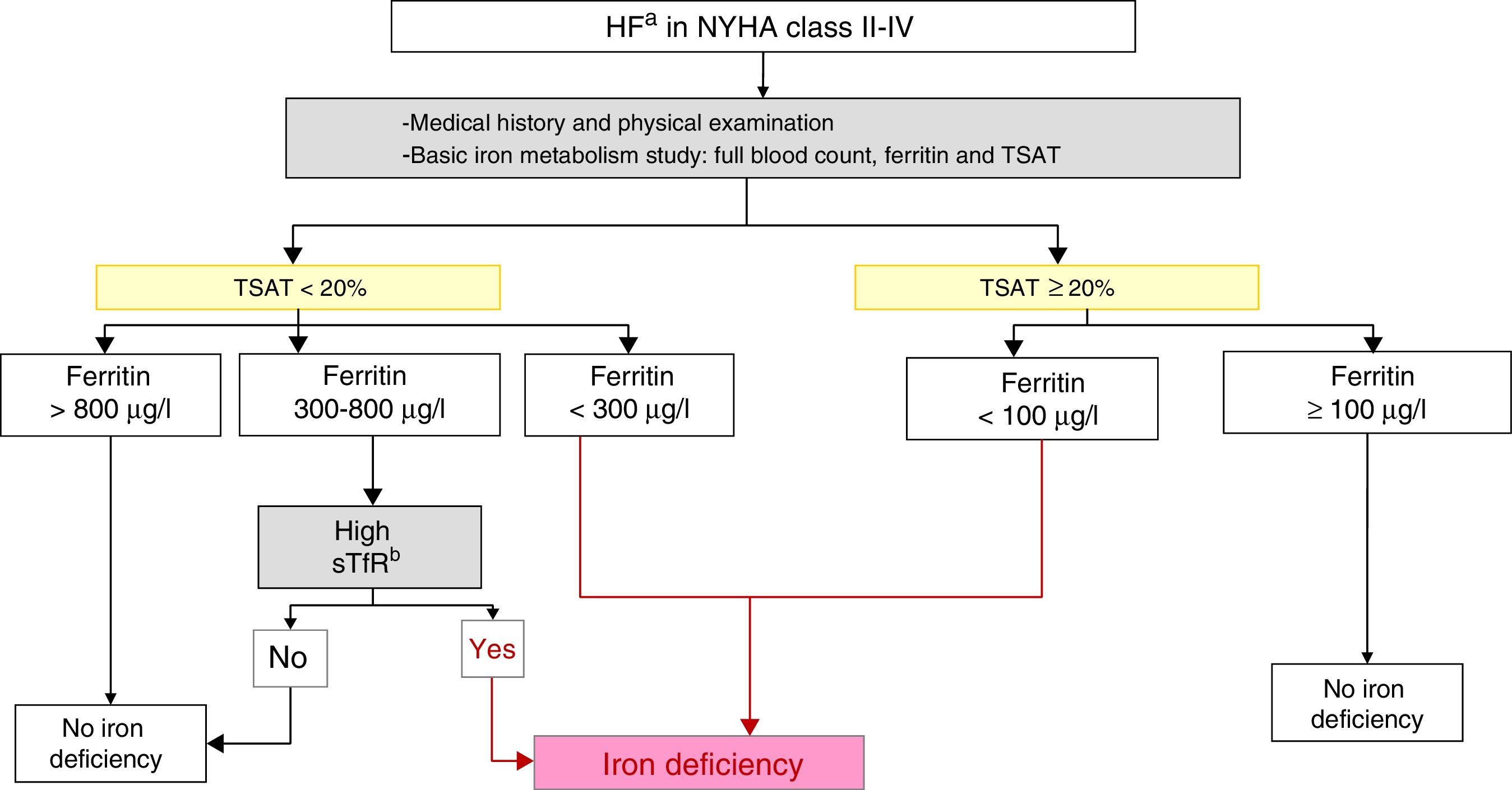
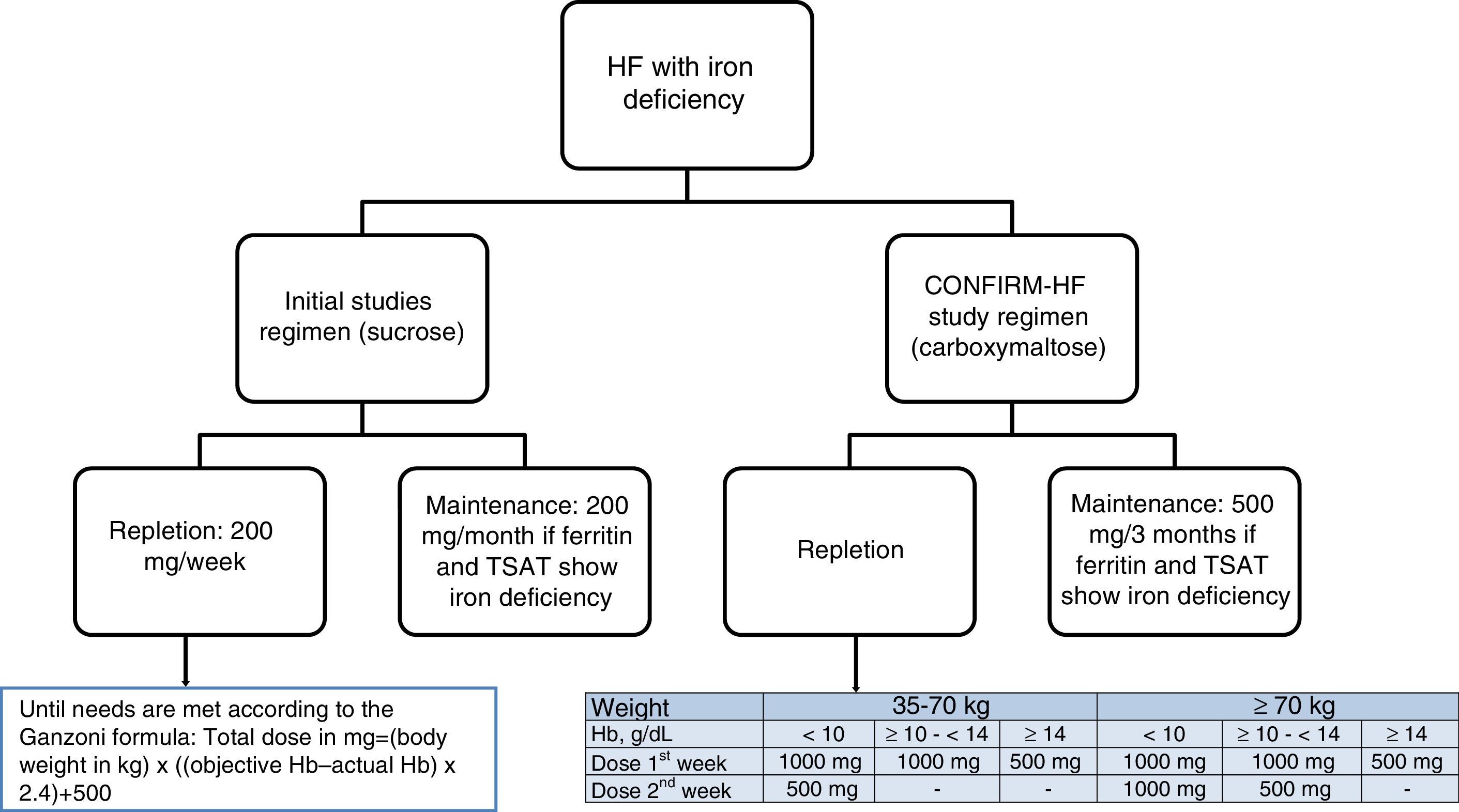
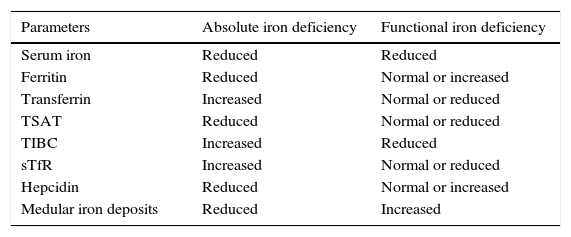
Iron deficiency in patients with heart failure is a medical problem of recent particular interest. This interest has resulted from the publication of several clinical trials that demonstrated that the administration of intravenous iron to such patients improved their functional capacity and even reduced the number of hospitalisations for heart failure decompensation. However, applying the evidence from these studies in clinical practice is still controversial, both in terms of the diagnostic criteria for iron deficiency (absolute and functional) and the optimal method for iron replenishment. This article is a consensus document that integrates the recommendations of the Spanish Society of Internal Medicine and the Spanish Society of Cardiology. The article reviews the scientific evidence and proposes a diagnostic and therapeutic performance protocol for iron deficiency in heart failure.
El déficit de hierro en los pacientes con insuficiencia cardiaca es un problema médico que últimamente suscita un interés particular. Esto se debe a la publicación de varios ensayos clínicos que demuestran que la administración de hierro intravenoso en estos pacientes mejora su capacidad funcional, e incluso reduce los ingresos por descompensación de insuficiencia cardiaca. Sin embargo, la aplicación de la evidencia aportada por estos estudios en la práctica clínica es aún controvertida, tanto en los criterios diagnósticos del déficit de hierro, absoluto y funcional, como en la forma óptima de reposición del hierro. Este artículo es un documento de consenso que integra las recomendaciones de las Sociedades Españolas de Medicina Interna y Cardiología en el que se revisa la evidencia científica y se propone un protocolo de actuación diagnóstica y terapéutica del déficit de hierro en la insuficiencia cardiaca.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<