Burnout is a psychosocial syndrome caused by stressful situations in the workplace. It affects 30%–60% of medical professionals. The aim of this study is to carry out a comparative analysis of its frequency before and after the COVID-19 outbreak in Spanish internal medicine attending physicians.
MethodsSurveys that included the Maslach Burnout Inventory were sent via email and associated social networks to physicians who were members of the Spanish Society of Internal Medicine in 2019 and 2020.
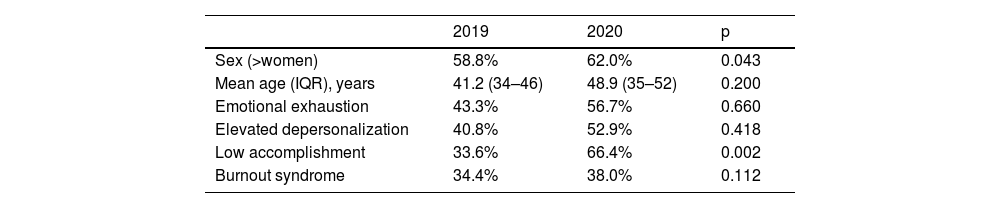
ResultsA non-significant increase in burnout was observed (38.0% vs. 34.4%). However, an increase in low personal fulfilment was observed (66.4% vs. 33.6%; p = 0.002), a dimension associated with the prevention of psychiatric morbidity, in addition to two others: emotional fatigue and depersonalization, which can negatively affect patient care.
ConclusionsIt is essential to address this syndrome individually and institutionally.
El burnout es un síndrome psicosocial causado por situaciones estresantes en el ámbito laboral. Afecta al 30-60% de los profesionales médicos. El objetivo de este estudio es realizar un análisis comparativo de su frecuencia antes y después del brote de la COVID-19 en los médicos adjuntos de Medicina Interna españoles.
MétodosSe enviaron encuestas por correo electrónico y redes sociales integradas con el Maslach Burnout Inventory a los miembros de la Sociedad Española de Medicina Interna en 2019 y 2020.
ResultadosSe ha observado un aumento no significativo de burnout (38,0% vs. 34,4%). Sin embargo, sí se constata un aumento en la baja realización personal (66,4% vs. 33,6%; p = 0,002), dimensión asociada a la prevención de la morbilidad psiquiátrica, además de otras dos: la fatiga emocional y la despersonalización, que pueden afectar negativamente a la atención del paciente.
ConclusionesEs esencial abordar este síndrome individual e institucionalmente.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<