The study aimed to describe patient characteristics and outcomes by PaO2/FiO2 (PAFI) and degree of inflammation.
MethodsRetrospective cohort study with data on patients collected from March 1st, 2020 to March 1st, 2023, from the Spanish SEMI-COVID-19 Registry. Non-nosocomial patients with data on PAFI (<100 vs. 100−200 vs. 200−300 vs. >300) who received corticosteroids (CS) for COVID-19 in the first 48&#¿;h of admission were included in the study. 5314 patients met the inclusion criteria for the present study. The primary outcome was in-hospital mortality.
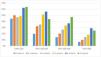
ResultsHigher in-hospital mortality was found in the groups with PAFI&#¿;<&#¿;100 (51.5% vs. 41.2% vs. 25.8% vs. 12.3%, P&#¿;<&#¿;.001). They also required more NIMV, IMV, and ICU admission, and had longer hospital stays. Those patients with PAFI&#¿;>&#¿;300 and 4–5 high-risk criteria presented higher mortality than the patients with PAFI 200−300 and only 1−2 criteria of analytical inflammation. Risk factors associated with higher in-hospital mortality were age [OR&#¿;=&#¿;1.06 (1.05−1.06)], moderate [OR&#¿;=&#¿;1.87 (1.49−2.33)] and severe [OR&#¿;=&#¿;2.64 (1.96−3.55)] degree of dependency, dyslipidemia [OR&#¿;=&#¿;1.20 (1.03−1.39)], higher Charlson index [OR&#¿;=&#¿;1.19 (1.14−1.24)], tachypnea on admission [2.23 (1.91−2.61)], the higher number of high-risk criteria on admission, and lower PAFI on admission. Female gender [OR&#¿;=&#¿;0.77 (0.65−0.90)] and the use of RDSV [OR&#¿;=&#¿;0.72 (0.56−0.93)] were found to be protective factors.
ConclusionsThe lower the PAFI and the higher the degree of inflammation in COVID-19, the higher the in-hospital mortality. Inflammatory escalation precedes respiratory deterioration and should serve as an early predictor of severity to deciding the use of anti-inflammatory/immunosuppressive therapy.
El estudio tenía como objetivo describir las características y los resultados de los pacientes según la PaO2/FiO2 (PAFI) y el grado de inflamación.
MétodosEstudio de cohortes retrospectivo con datos de pacientes recogidos desde el 1 de marzo de 2020 hasta el 1 de marzo de 2023, del Registro Español SEMI-COVID-19. Se incluyeron en el estudio pacientes no nosocomiales con datos de PAFI (<100 vs 100−200 vs 200−300 vs >300) que recibieron corticoides (CS) por COVID-19 en las primeras 48&#¿;h de ingreso. 5.314 pacientes cumplieron los criterios de inclusión para el presente estudio. El resultado primario fue la mortalidad intrahospitalaria.
ResultadosSe encontró mayor mortalidad intrahospitalaria en los grupos con PAFI&#¿;<&#¿;100 (51,5% vs 41,2% vs 25,8% vs 12,3%, P&#¿;<&#¿;,001). También requirieron más VMNI, VMI e ingreso en UCI, y tuvieron estancias hospitalarias más prolongadas. Los pacientes con PAFI&#¿;>&#¿;300 y 4–5 criterios de alto riesgo presentaron mayor mortalidad que los pacientes con PAFI 200−300 y sólo 1−2 criterios de inflamación analítica. Los factores de riesgo asociados a una mayor mortalidad intrahospitalaria fueron la edad [OR&#¿;=&#¿;1,06 (1,05–1,06)], el grado de dependencia moderado [OR&#¿;=&#¿;1,87 (1,49–2,33)] y grave [OR&#¿;=&#¿;2,64 (1,96–3,55)], la dislipidemia [OR&#¿;=&#¿;1, 20 (1,03–1,39)], mayor índice de Charlson [OR&#¿;=&#¿;1,19 (1,14–1,24)], taquipnea al ingreso [2,23 (1,91–2,61)], mayor número de criterios de alto riesgo al ingreso y menor PAFI al ingreso. El sexo femenino [OR&#¿;=&#¿;0,77 (0,65–0,90)] y el uso de RDSV [OR&#¿;=&#¿;0,72 (0,56–0,93)] resultaron ser factores protectores.
ConclusionesA menor PAFI y mayor grado de inflamación en COVID-19, mayor mortalidad intrahospitalaria. La escalada inflamatoria precede al deterioro respiratorio y debería servir como predictor precoz de gravedad para decidir el uso de terapia antiinflamatoria/inmunosupresora.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<