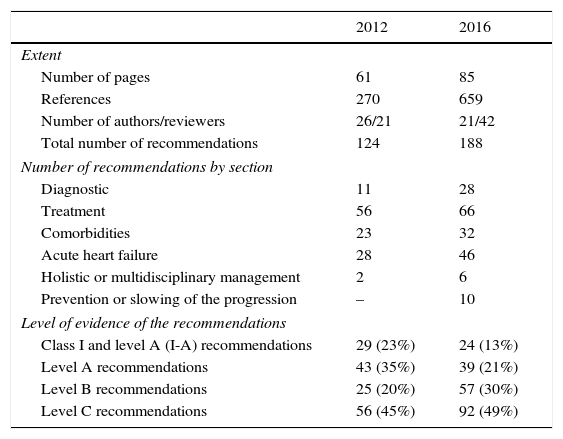
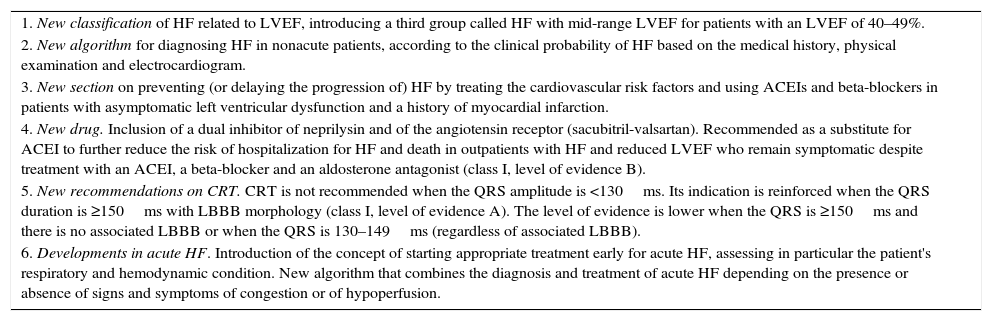
The European Society of Cardiology has recently published new guidelines on the diagnosis and treatment of acute and chronic heart failure (HF). This article aims to review these recommendations and their level of scientific evidence and to present the most innovative aspects. The most significant deviations from the 2012 edition are: (1) the introduction of the concept of HF with midrange LVEF (40–49%); (2) a new diagnostic algorithm for chronic HF, initially considering the clinical probability; (3) recommendations on preventing or delaying the apparition of HF; (4) indications for the use of the new sacubitril-valsartan compound, the first angiotensin receptor blocker and neprilysin inhibitor; (5) modification of indications for cardiac resynchronization therapy; and (6) a new algorithm for a combined diagnostic and treatment strategy for acute HF based on the presence or absence of congestion and hypoperfusion.
Recientemente se han publicado las nuevas guías sobre diagnóstico y tratamiento de la insuficiencia cardiaca (IC) aguda y crónica de la Sociedad Europea de Cardiología. El objetivo de este artículo es revisar estas recomendaciones, su nivel de evidencia científico y los aspectos más novedosos. Los cambios más importantes con respecto a la edición de 2012 se refieren a: 1) introducción del concepto de IC con fracción de eyección en rango medio (40–49%); 2) nuevo algoritmo diagnóstico de la IC crónica considerando inicialmente la probabilidad clínica; 3) recomendaciones para prevenir o retrasar la aparición de IC; 4) indicaciones para el uso del nuevo compuesto sacubitrilo-valsartán, el primer inhibidor del receptor de la angiotensina y neprilisina; 5) modificación de las indicaciones para la terapia de resincronización cardiaca; y 6) nuevo algoritmo para una estrategia combinada de diagnóstico y tratamiento de la IC aguda según la presencia o ausencia de congestión e hipoperfusión.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<