Hypertension (HT) is one of the main risk factors for cardiovascular disease (CVD). Although it is a global problem, independently of economic situation, region, race or culture, the data available on Latin America are limited. Clinical guidelines emphasise the importance of obtaining reliable blood pressure readings. For this reason, the use of ambulatory blood pressure monitoring (ABPM) is recommended. This improves precision and reproducibility, resulting in better diagnosing and therapeutic decision-making, and constitutes a better estimation of prognosis than office measurements.
Unfortunately, there is no global prospective ABPM registry for all of Latin America that analyses HT prevalence, the level of knowledge about it, treatment percentage and the degree of control. Consequently, the authors of this article consider its implementation a priority.
La hipertensión arterial (HTA) es el principal factor de riesgo de enfermedad cardiovascular (ECV). Aunque es un problema global, independiente de la situación económica, región, raza o cultura, los datos disponibles con respecto a Latinoamérica no son muy abundantes. Por otra parte, las guías clínicas enfatizan la importancia de obtener lecturas fiables de la presión arterial. Por ello, se recomienda el uso de la monitorización ambulatoria de la presión arterial (MAPA) que mejora su precisión y reproducibilidad, ayudando a un mejor diagnóstico, en la toma de decisiones terapéuticas, y representa una mejor estimación pronóstica que las medidas en consulta.
Lamentablemente, no existe ningún registro prospectivo global de MAPA para toda Latinoamérica, que analice la prevalencia de HTA, el grado de su conocimiento, su porcentaje de tratamiento y el grado de control. En consecuencia, los autores de este artículo consideran prioritaria su puesta en marcha.
Arterial hypertension (HTN) is the principal risk factor for cardiovascular disease (CVD) and affects a portion of the population equivalent to 22.3% globally and 26.5% in middle income countries, a category which includes Latin American countries1. Starting at 115/75 mmHg, an increase of 20 mmHG in systolic blood pressure (SBP) or of 10 mmHG in diastolic blood pressure (DBP) is associated a twofold risk of CVD2.
In a systematic analysis of 87 cardiovascular (CV) risk factors, carried out in the population of 204 countries in the period spanning 1990–2019, HTN, defined as persistent elevation of blood pressure levels (BP) ≥ 140/90 mmHg, was the main factor for mortality globally, representing a total of 10.8 million out of all the deaths from the year 20193.
While it has been clearly confirmed that this is a global problem4, independent of the economic situation5, region, race, or culture, the data available on Latin American (LATAM) countries are limited.
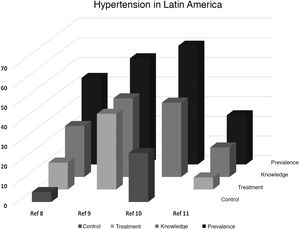
HTN situation in Latin AmericaIn LATAM countries, HTN has been calculated to be responsible for 1.6 million annual deaths due to CVD, of which 500,000 occur before the age of 706. Similarly, HTN is the main risk factor for coronary artery disease (CAD) and cerebrovascular disease (CVD), which affect between 20 and 40% of Latin American adults6,7. Nevertheless, in terms of LATAM, the available data are scarce and not readily accessible (Fig. 1).
The published data show a situation that is far from adequate. One recent cross-sectional study including 33,276 individuals (average age of 52 years and 60% women) from urban (68%) and rural communities (32%) from 6 countries from Latin America (Argentina, Brazil, Chile, Colombia, Peru and Uruguay), reported a prevalence of HTN of 44%, defined according to the criteria of the Latin American Guidelines on Hypertension (BP ≥ 140/90 mmHg). Although 58.9% of the patients were aware of their HTN diagnosis, only 53.3% received treatment and, of those, only 37.6% had their HTN under control (BP < 140/90 mmHg)8.
On the other hand, the initiative May Measurement Month (MMM,) from 2017 performed a cross-sectional survey of individuals over the age of 18, implemented in 18 LATAM countries and the Caribbean, which included a total of 105,246 individuals with an average age of 48.6, and showed that 42,328 (40.4%) were hypertensive. In addition, the prevalence of other CV risk factors was higher in the hypertensive subjects9.
In the Venezuelan Study of Cardio-Metabolic Health (EVESCAM according to the Spanish acronym)10, which performed a randomised, cross-sectional, cluster sampling representative of the national Venezuelan population, the crude incidence of HTN11, according to the 2017 AHA/ACC guidelines criteria, was 60.4%. The prevalence of uncontrolled BP (≥130/80 mmHg) in subjects with a HTN diagnosis and antihypertensive therapy was 66.8% in men and 65.8% in women. According to this study, the total estimated number of individuals with HTN in Venezuela is 11 million, of which only about 1.8 million are controlled.
In Brazil12, the current estimated prevalence of HTN is 32.3% and the BP control rate in cardiologist-treated patients is 60.6%13,14, with no significant differences perceived between ethnicities.
In Mexico, over the past 20 years, 5 national probabilistic surveys (ENSA 2000, ENASANUT 2006, 201214, 201615 and 2018-1916) and 2 opportunistic surveys, MMM-18 and MMM-1917, have been carried out which included information on HTN, its prevalence, prior knowledge, treatment, and goal attainment for HTN in the country. The data from the probability surveys show that the prevalence of HTN (BP ≥140/90 mmHg) decreased from 31.6% in 2012 to 25.5% in 2016, likely due to use of automated BP equipment in the second survey. However, the proportion of previous knowledge increased, being 39, 50, and 60 in the 3 subsequent surveys (2006, 2012 and 2016).
Of the 39,700 participants in the MMM-19 survey, it was observed that 10,140 (25.5%) were hypertensive and of these, 43.8% were aware of their disease. Of all the participants with HTN, only 41.7% were taking antihypertensive medication and of these, 4244 treated individuals, or 66.8%, had their BP under control (<140/90 mmHg). Regarding the type of treatment, 60% of the patients were receiving antihypertensive monotherapy; 20% dual therapy, and 10% triple therapy.
Other studies have been performed in specific populations or with different diagnostic criteria. Along these lines, a meta-analysis performed in Brazil evaluating the prevalence of HTN in indigenous populations showed a combined HTN prevalence of 6.2% in 1970, a figure that has been increasing annually by 0.7% from 1970 to 2014, reaching 30.1%18.
It is highly important to point out that there is very little data regarding prevalence, treatment, and control of the black population in Latin American countries and the Caribbean, or of the population that lives permanently at altitudes above 3000 m on the Andean Plateau.
What is more, the condition is considerably underdiagnosed in all of LATAM, with insufficient treatment and BP control, particularly in lower to middle income countries5. Therefore, there is a clear and urgent need to develop strategies to detect, prevent, treat, and control HTN in an effective manner throughout the entire continent.
Strategies to control HTN in Latin AmericaThe presented results demonstrate the high prevalence of HTN in LATAM, as well as the low rates of knowledge, treatment, and control which highlight the significance of HTN as a primary risk factor for CV disease and all-cause mortality19. As mentioned previously, all of this leads to the urgent need to develop strategies to prevent, detect, treat, and control HTN effectively in all countries, such as some of the innovative strategies that have been20 or are currently being tested out in certain countries in the region21.
The role of HTN is not just a mere cause of CV disease. Because it modulates its natural history, it constitutes a prognostic factor22,23 for the development of renal and CV diseases24,25.
Fortunately, it has been shown that reducing BP in hypertensive patients is accompanied by a reduction in the incidence of CV disease26. An inverse relationship between DBP and CAD has also been documented, with the presence of a J-shaped curve with little to no evidence that this J curve is present in brain or kidney complications. Regarding SBP levels, the presence of a J curve has not been shown in coronary, cerebrovascular or renal events27.
In the HOPE-3 study, 28% of the 12,500 subjects recruited were from different Latin American countries such as Argentina, Brazil, Colombia and Ecuador. This study, with a sample representative of the population of Latin America, showed that the reduction in BP with a standardised treatment consisting of a combination of half of the maximum dose of 2 antihypertensive medications (candesartan and hydrochlorothiazide) reduced the primary outcome comprised of CV death, myocardial infarction, and CVA only in individuals whose SBP was higher than 143 mmHg28.
Despite the recent publication of the Sprint study29, the benefit of intensive BP reduction has been reiterated. It is necessary to highlight that, at the moment, there is still some controversy surrounding intensive BP reduction in certain specific clinical situations, which is why achieving levels below 130/80 mmHg is not a general recommendation, but rather reserved for certain situations30.
Ambulatory measures for controlling HTN in Latin AmericaAll the current clinical guidelines emphasise the importance of obtaining reliable BP readings in patients with HTN and comorbidities7,20,24,25,31.
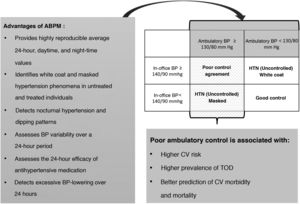
While the prognostic role of BP is undeniable in CVD32, we must keep in mind that the majority of available data are based on isolated brachial BP readings obtained in-office through conventional means, and these subject to wide variability due to the number of factors that influence this measurement. The use of self-measured BP (SMBP) at home improves precision and reproducibility33. The most recent clinical guidelines recommend more widespread use of outpatient measures, outside the physician’s office, both to confirm HTN diagnoses and to help with therapeutic decision-making during follow-up, via ambulatory BP monitoring during a 24-h period (ABPM) or via SMBP31. Fig. 2 summarises the recommendations and benefits of ABPM.
In addition, the currently available data suggest that ambulatory BP measurements represent a better prognostic estimation than in-office BP measurements31: both average levels during resting periods, typically at night, and the circadian rhythm of nocturnal dipping have a stronger association with target organ damage and CVD than clinical measurements31.
Among the differences found, it has been observed that the non-dipper night-time BP pattern is correlated with higher CV morbidity and mortality32. Similarly, in previously untreated patients with HTN, it has been observed that night-time BP levels measured by ABPM are a better predictor for CV, cerebrovascular, and renal events32.
The use of ambulatory BP measurements and their comparison with in-office BP measurements has made it possible to define situations in which the two disagree, both in untreated normotensive subjects and in hypertensive patients, which is known as isolated clinic HTN (white-coat HTN) and masked HTN (MHTN)31. The first consists of elevated in-office BP with normal ambulatory measurements, while the second is defined as the presence of persistently normal BP figures in-office with ambulatory levels that are in the hypertensive range (Fig. 2). What is more, ambulatory BP measurements in treated subjects make it possible to detect the presence of uncontrolled MHTN (MHTN situation in treated patients) and its prevalence (11.1%), as well as the presence of uncontrolled isolated clinic HTN (white-coat HTN in treated patients) and its prevalence (15.4%). These 2 situations are frequent and only detectable through joint use of in-office and ambulatory measurements.
The importance of detecting masked HTN situations lies in its association with higher CV risk33,34 and a higher prevalence of target organ damage35, meaning the use of ambulatory BP measurement improves the prediction of CV morbidity and mortality35–38. As has been described, this particularly important aspect shows higher morbidity and mortality in patients with nocturnal HTN31, and it is important to remember that this condition is only detectable via the use of ABPM (Fig. 2).
The different prevalence of MHTN reported by various authors is due to the fact that different clinical situations have been included interchangeably within this term. Those situations correspond to both treated and untreated patients as well as normotensive subjects without treatment who present BP levels via ABPM that exceed the normal limits.
On the other hand, multiple published studies have used different definitions for good control of ambulatory BP through the use of different reference periods for the normal rhythm, either the 24-h period, active period, or resting period. In addition, it is possible that the methodology for measuring BP in-office has also influenced the reported results.
Therefore, it is necessary to standardise the methodology for measuring BP via ABPM and SMBP.
Final reflectionUnfortunately, these data are not available for analysis in the Latin American population as to date, no global prospective registry has been created that gathers information for all of LATAM, including HTN prevalence, the level of knowledge among the actual patients, the number of patients in treatment, and the number of controlled hypertensive individuals.
Only the Artemis registry, which analysed data from 14,143 patients from 27 countries from the 5 continents, included data from 1273 individuals from the American continent (Argentina, Brazil, Canada, Mexico and Venezuela)39.
Consequently, the authors of this article consider it a priority to create a Latin American ABPM registry to analyse, among other variables: the influence of factors such as average daytime and night-time SBP and DBP levels; the circadian rhythm of both BP components; the BP model of change during sleep compared to wakefulness, or the BP change profile during the waking hours of the population; and across the different geographic areas, ethnicities, social classes, etc.
The registry should also make it possible to evaluate the efficacy of the different antihypertensive therapy strategies and their long-term impact on reducing cardio-cerebral-renal-vascular outcomes.
The current existence of networks involving professionals from various Latin American countries with positive experience in prior collaboration projects guarantees the feasibility of immediate implementation of the registry in order to solve this urgent need.
FundingNone.
Conflicts of interestThe authors declare they have no conflicts of interest.
Please cite this article as: Camafort M, Alcocer L, Coca A, Lopez-Lopez JP, López-Jaramillo P, Ponte-Negretti CI, et al. Registro Latinoamericano de monitorización ambulatoria de la presión arterial (MAPA-LATAM): una necesidad urgente. Rev Clin Esp. 2021;221:547–552.