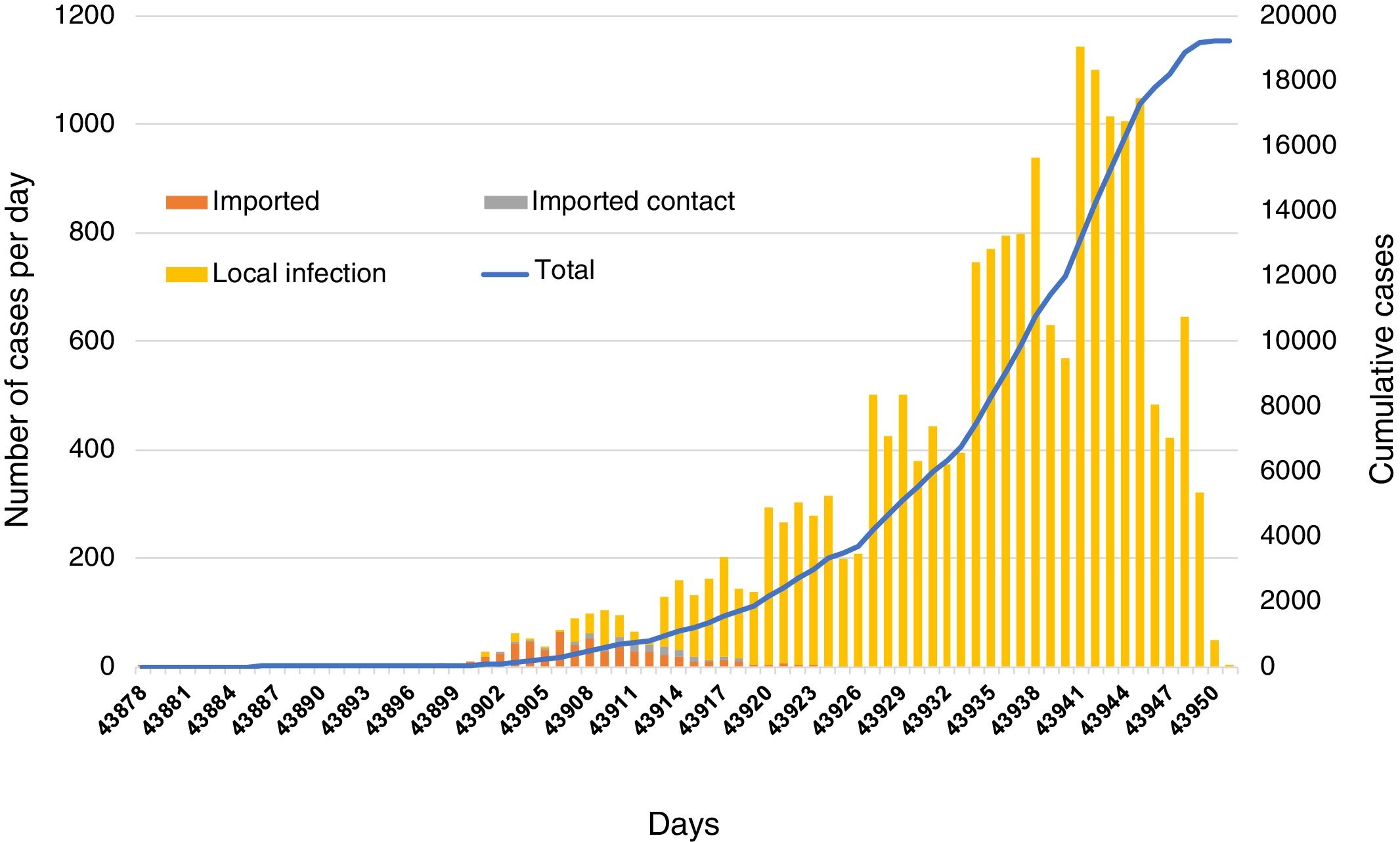
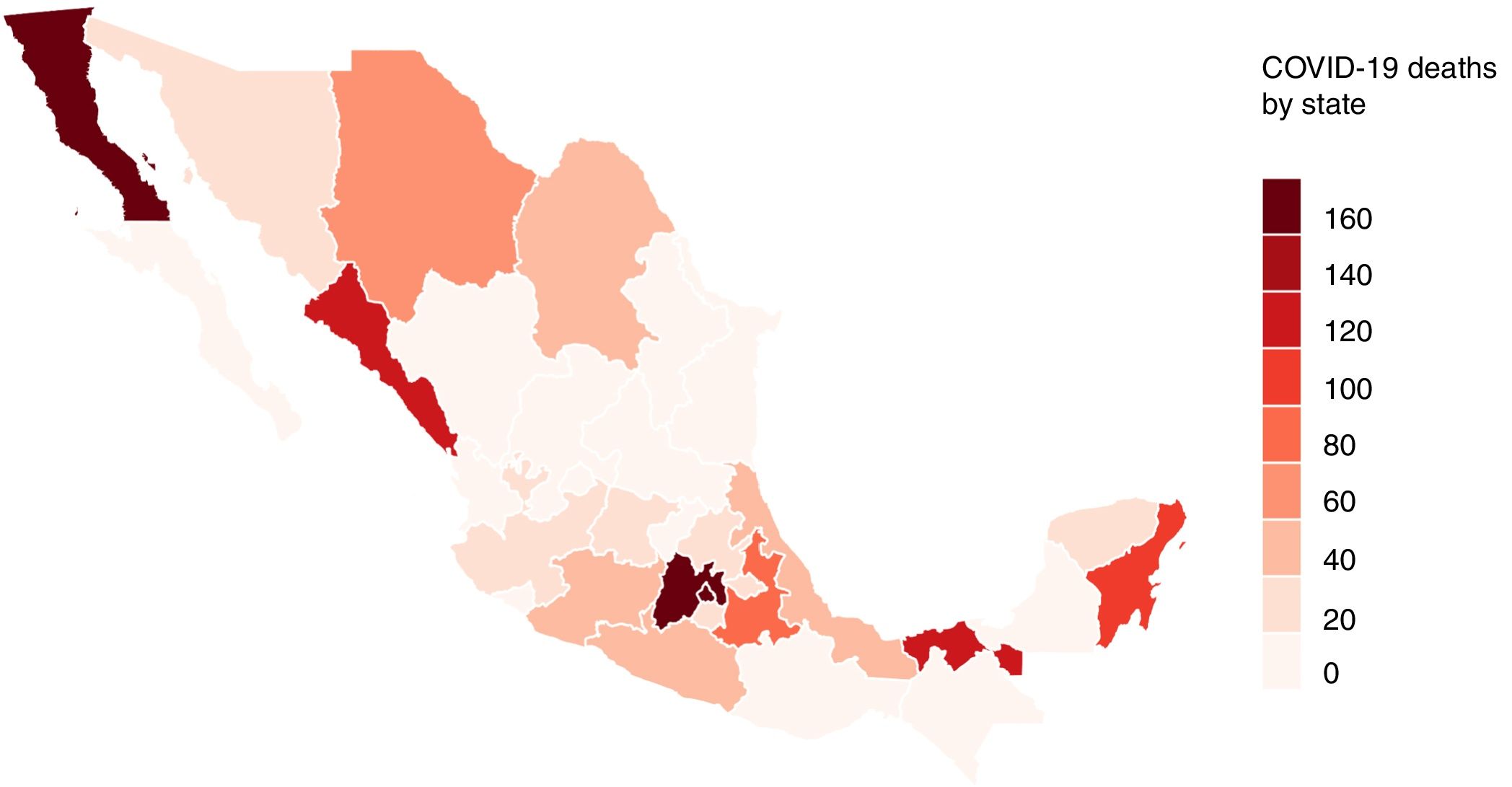
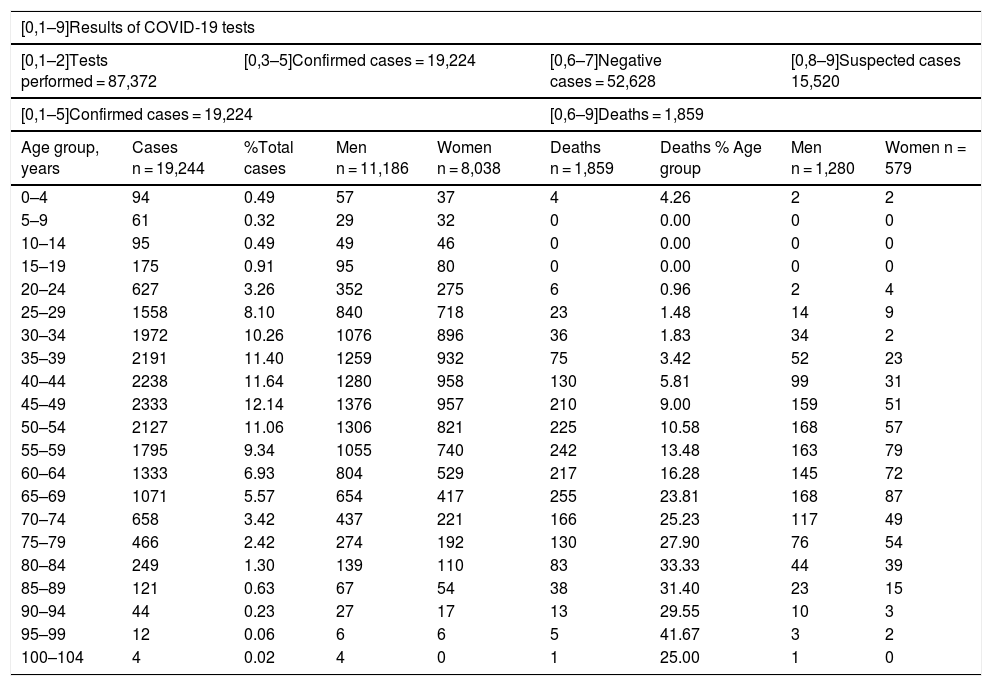
The first case of COVID-19 detected in Mexico was on the 27th of February 2020. On the 30th of April, 64 days after this first diagnosis, the number of patients had increased exponentially, reaching 19,224 confirmed cases and 1859 (9.67%) deaths. In response to this global outbreak, we summarize the current state of our understanding regarding COVID-19 in Mexico.
MethodsWe obtained the data from the official website of the Ministry of Health in Mexico. The study period covered the 27th of February to the 30th of April 2020. The cases were confirmed using real-time reverse transcription-polymerase chain reaction assays, and we analyzed the epidemiological, demographic and clinical data.
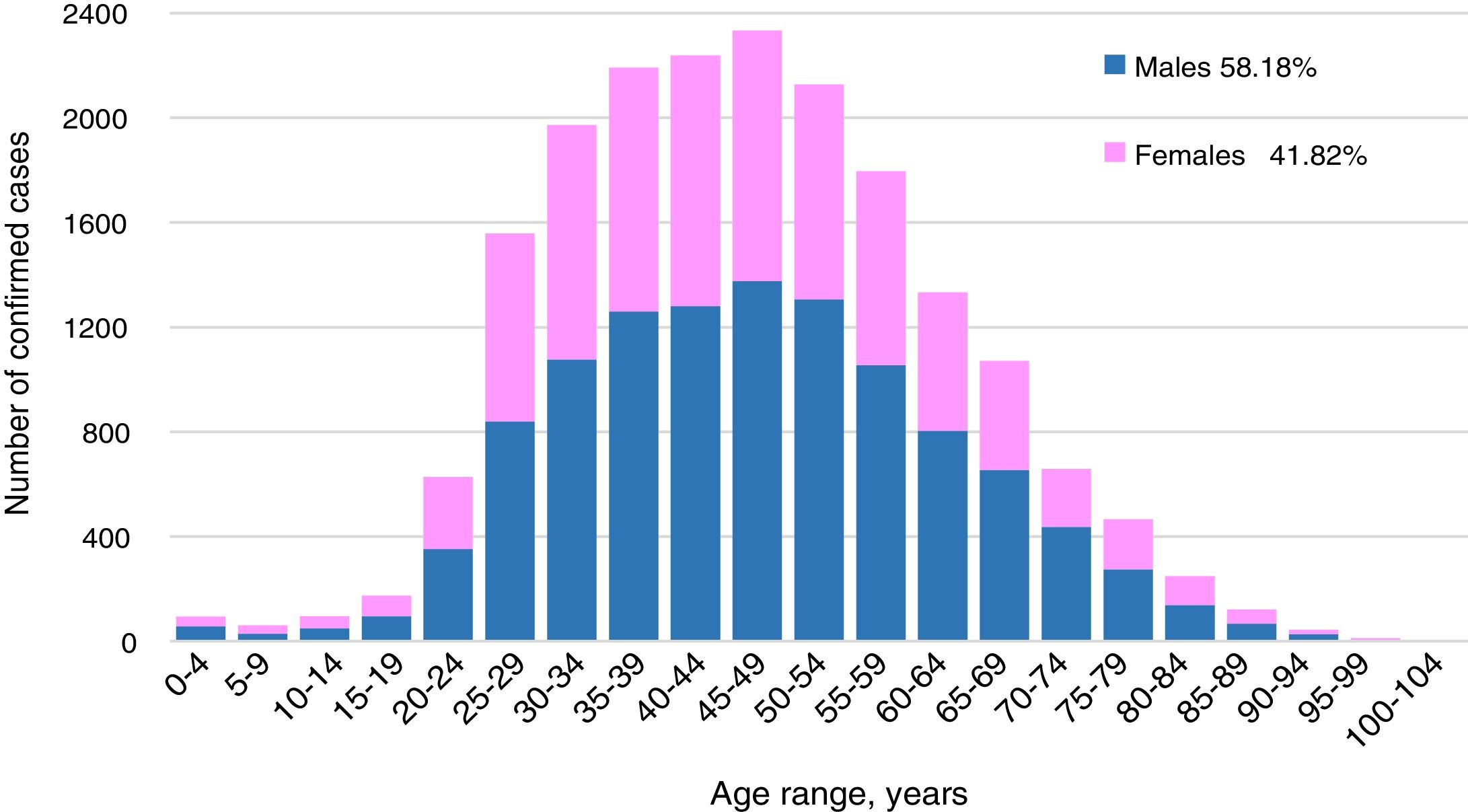
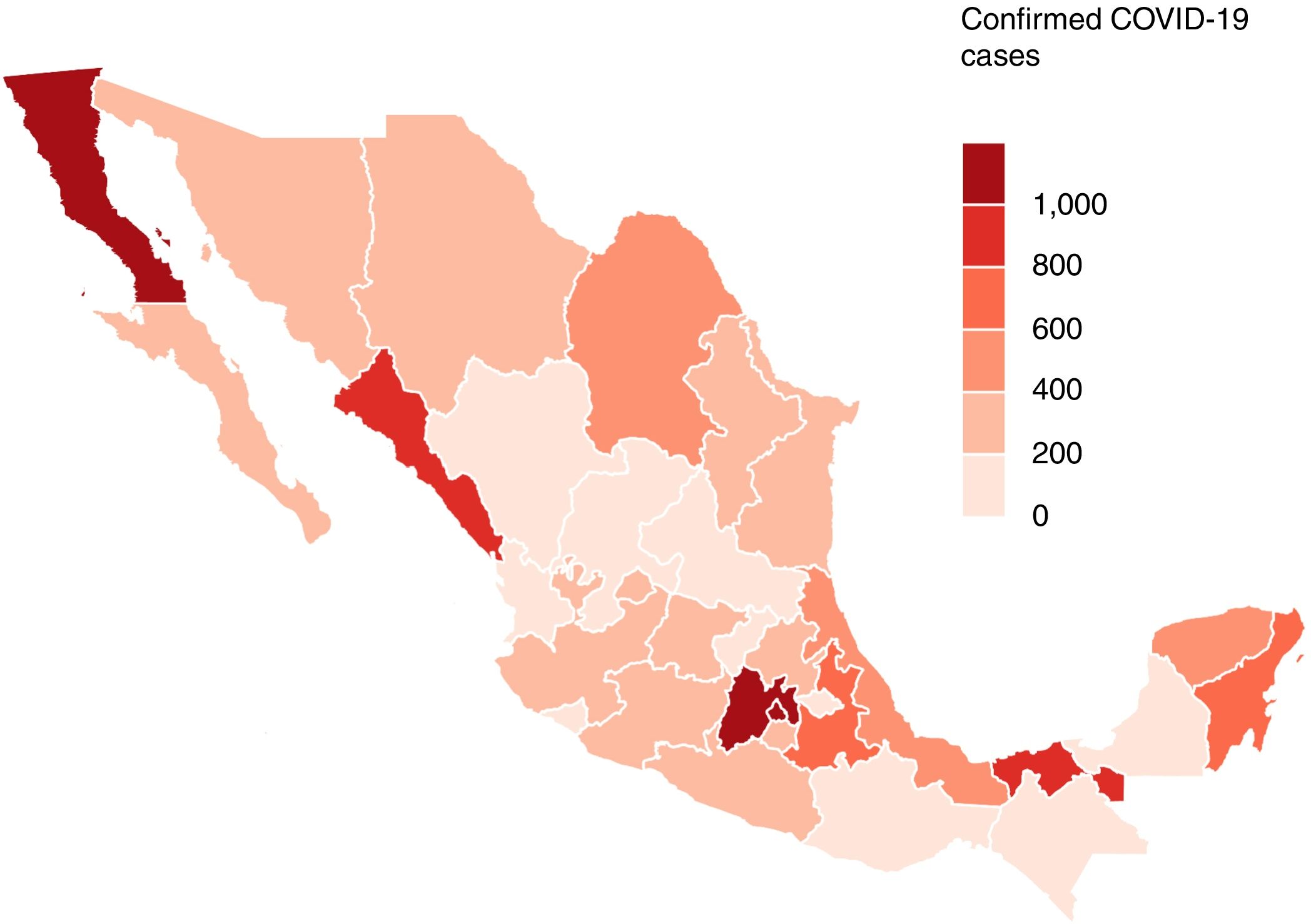
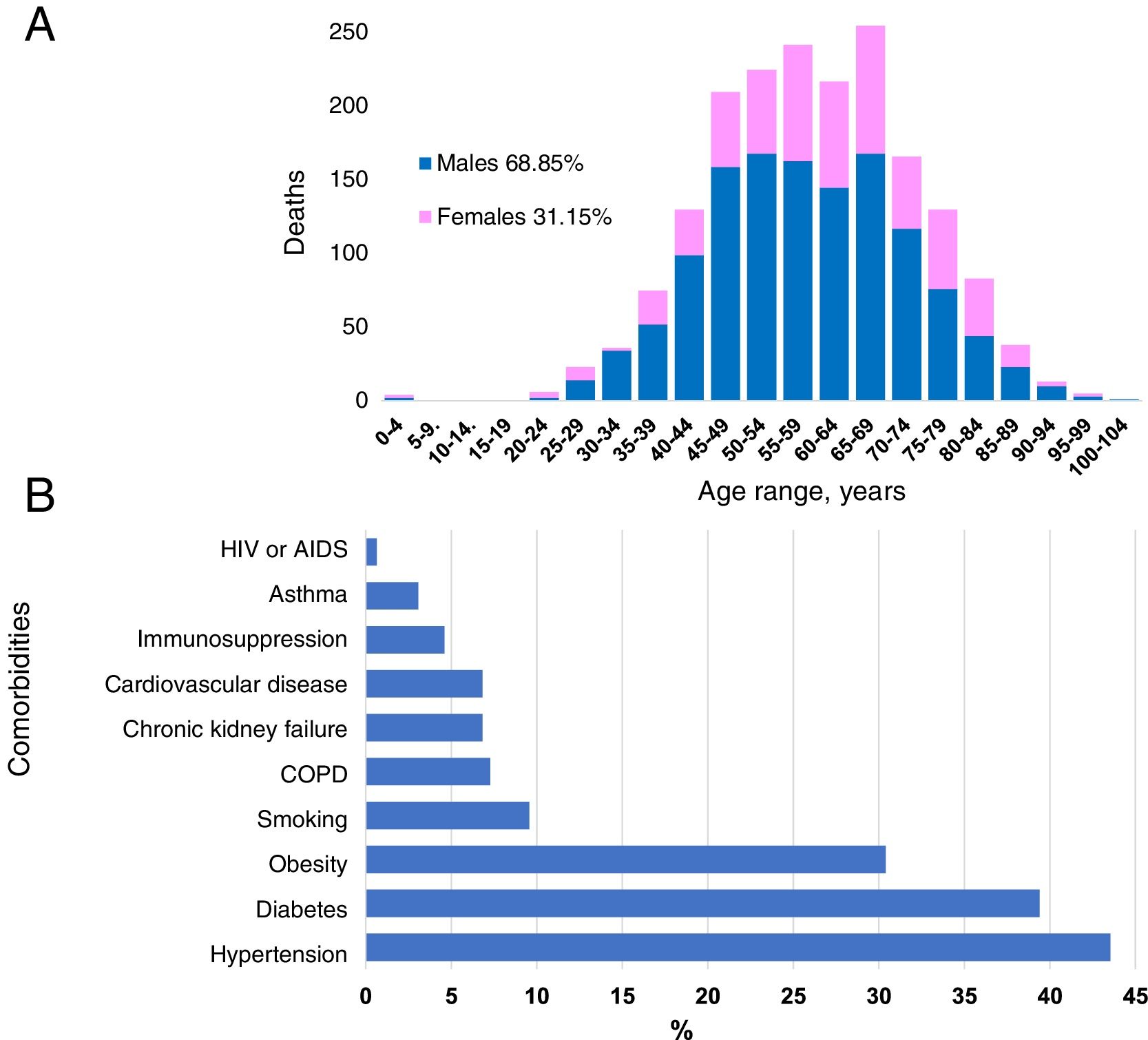
ResultsIn Mexico, most cases of COVID-19 were located in Mexico City. The mean age of the patients was 46 years. Of the 12,656 confirmed cases, most infected individuals were between the ages of 30 and 59 years (65.85%), and there was a higher incidence rate for men (58.18%) than for women (41.82%). The patients who died had one or more comorbidities, mainly hypertension (45.53%), diabetes (39.39%) and obesity (30.4%). In the first 64 days of the epidemic, China had reported 80,304 cases, with a mortality rate of 3.66%.
ConclusionsOur results indicate the early transmission of COVID-19 in Mexico. The descriptive epidemiology shows similarities between the cases of COVID-19 in Mexico and those in China. In the same period of the epidemic curve, we observed a reduction in the number of confirmed cases of COVID-19 in Mexico and a higher mortality rate compared with that of China.
El primer caso de COVID-19 se detectó en México el 27 de febrero de 2020. El 30 de abril, 64 días después de este primer diagnóstico, el número de pacientes aumentó exponencialmente, alcanzando un total de 19.224 casos confirmados y 1.859 (9,67%) fallecidos. En respuesta a este brote global, resumimos el estado actual del conocimiento sobre COVID-19 en México.
MétodosLos datos se obtuvieron del sitio web oficial del Ministerio de Salud en México. El período analizado fue entre el 27 de febrero y el 30 de abril de 2020. Los casos se confirmaron mediante RT-PCR en tiempo real y se analizaron los datos epidemiológicos, demográficos y clínicos.
ResultadosLa mayoría de los casos de COVID-19 se ubicaron en la Ciudad de México. La edad promedio de los pacientes fue de 46 años. De los 12.656 casos confirmados, el mayor número de infectados ocurre en el rango de edad entre 30 y 59 años (65,85%), y hubo una mayor incidencia en hombres (58,18%) que en mujeres (41,82%). Los pacientes fallecidos tenían una o múltiples comorbilidades, principalmente hipertensión (45,53%), diabetes (39,39%) y obesidad (30,4%). En los primeros 64 días de epidemia, China había reportado 80.304 casos con una tasa de mortalidad del 3,66%.
ConclusionesNuestros resultados indican la transmisión temprana de COVID-19 en México. La epidemiología descriptiva muestra las similitudes entre los casos de COVID-19 de México y China. En el mismo período de la curva epidémica, observamos en México una reducción en el número de casos confirmados de COVID-19 y una mayor tasa de mortalidad en comparación con China.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.
Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<