To analyze the care received by patients with type 2 diabetes mellitus (DM2) and comorbidity in Spain's National Health System.
Patients and methodsCross-sectional study using an online survey. A total of 302 family physicians, internists and endocrinologists participated in the study. The participants were recruited voluntarily by their respective scientific societies and received no remuneration.
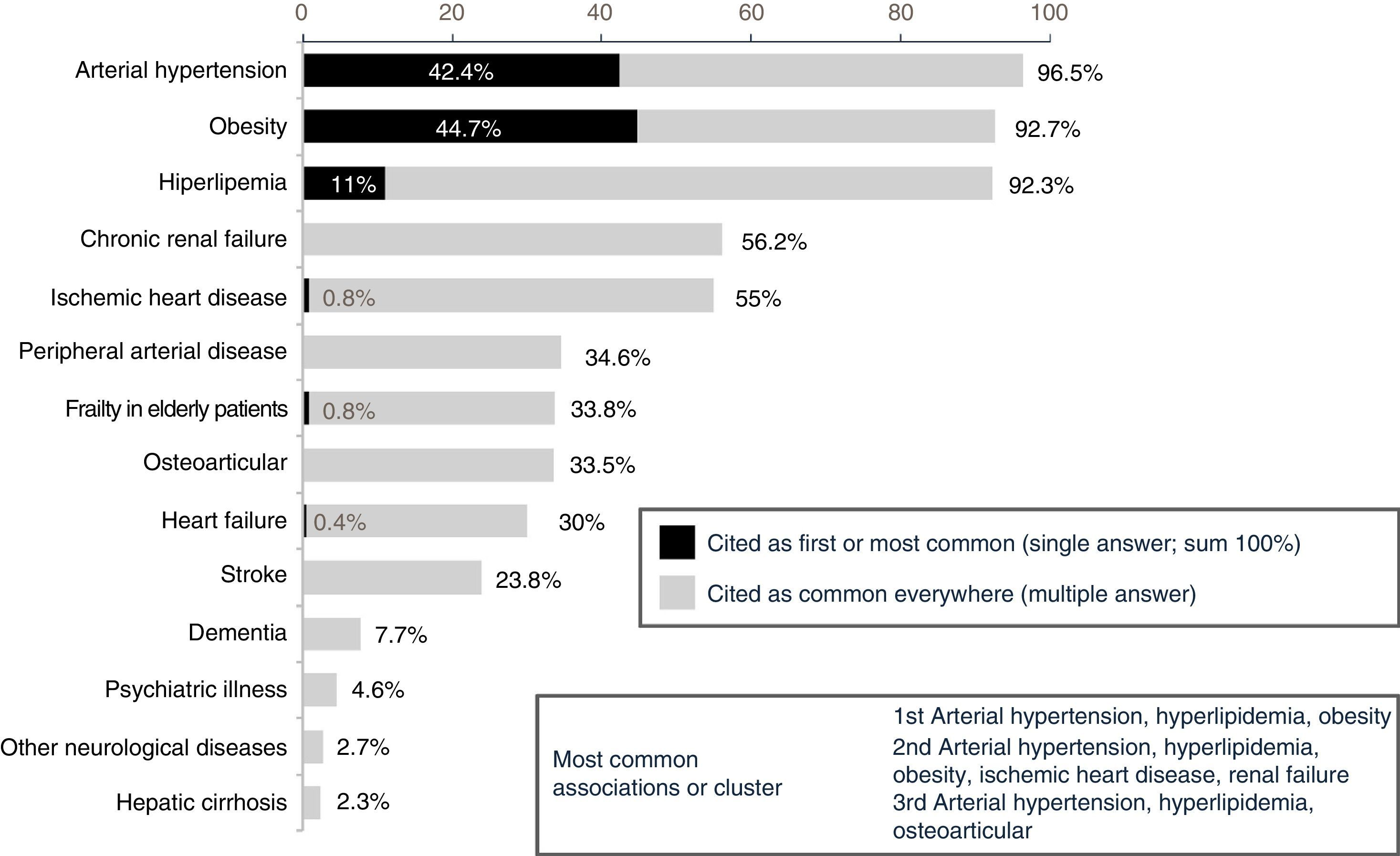
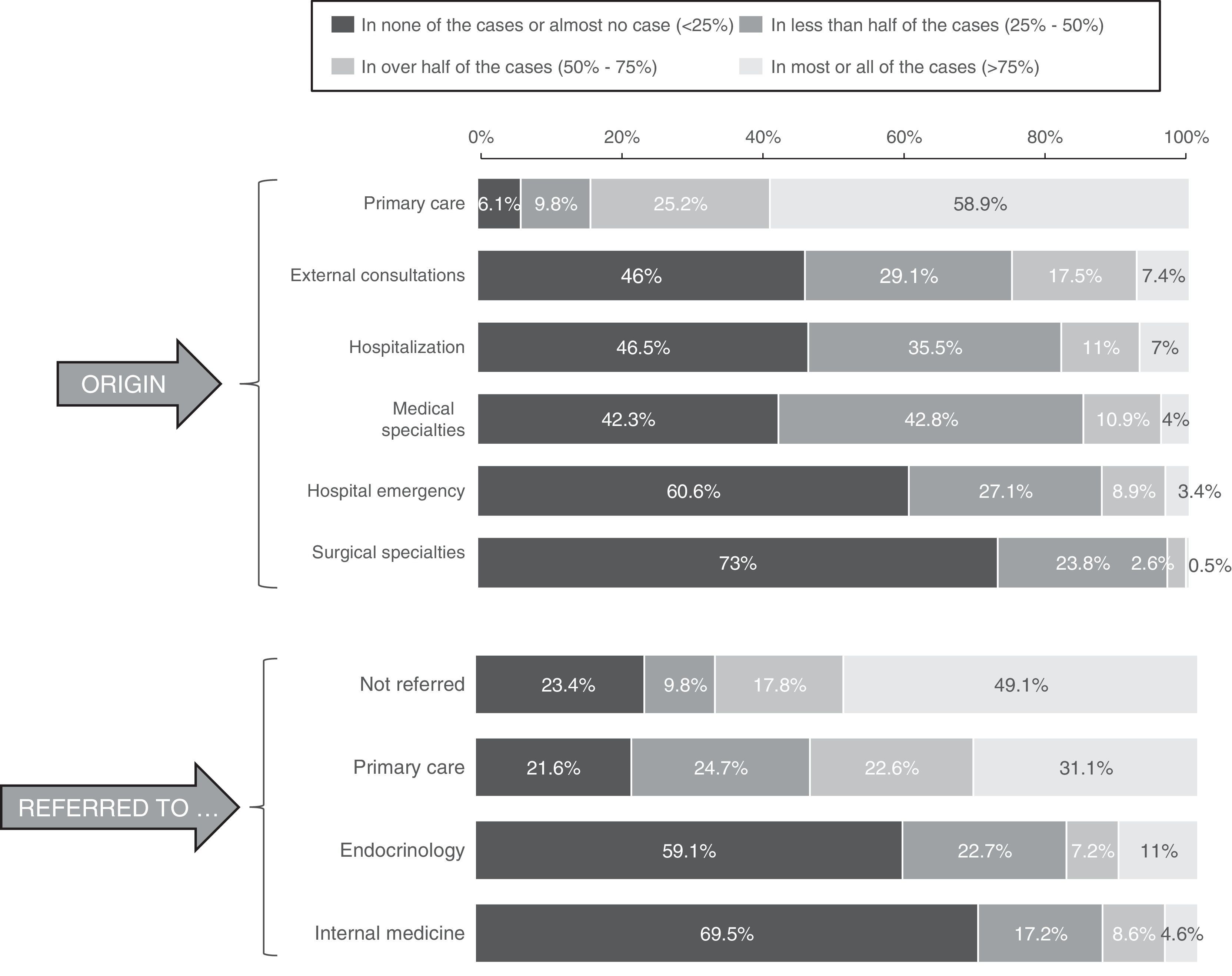
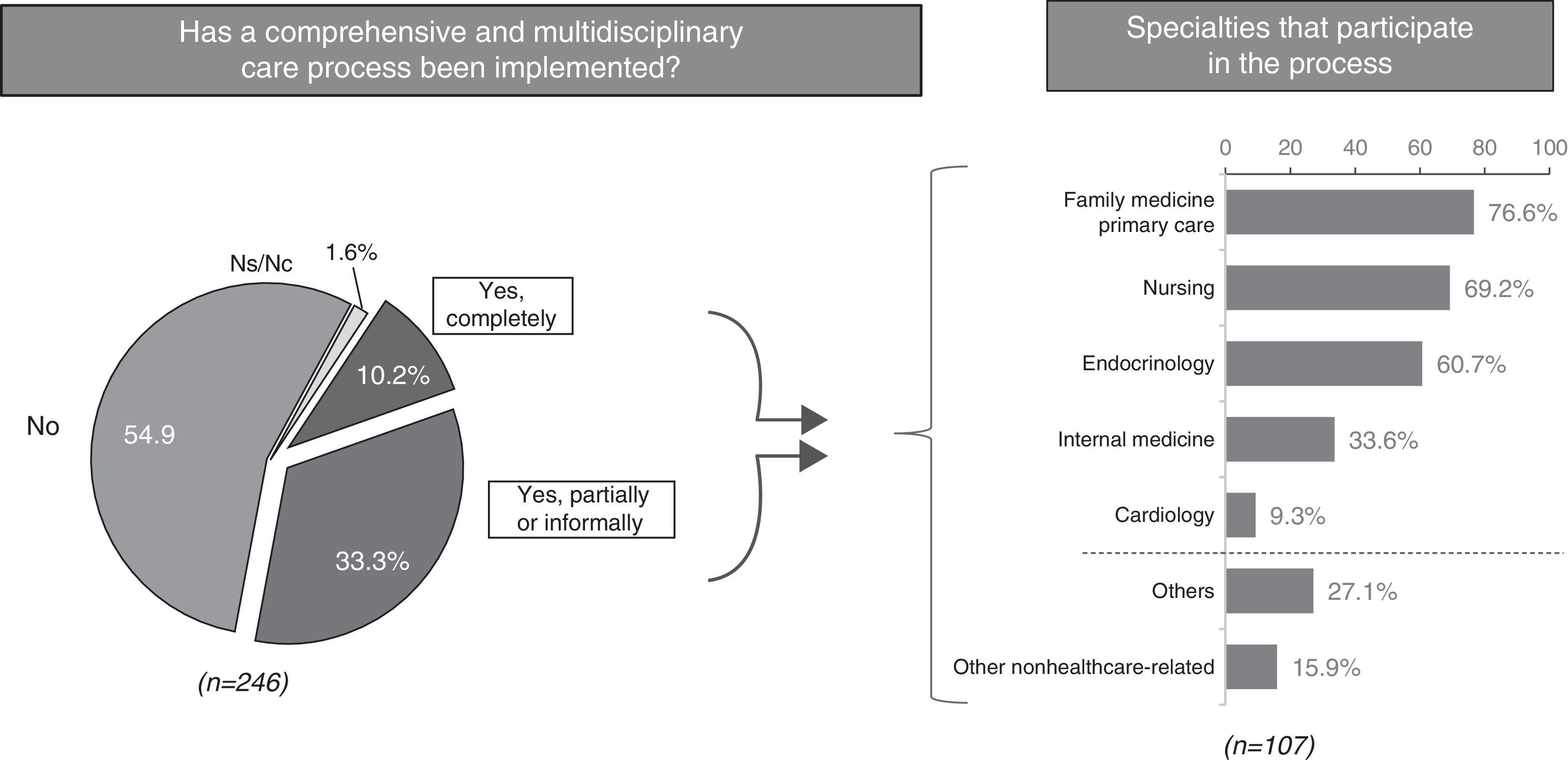
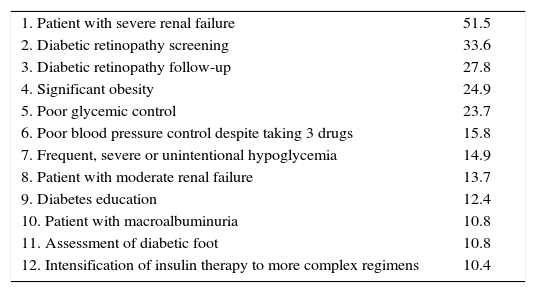
ResultsPatients with DM2 and comorbidity are mostly treated in Primary Care (71.8%). Forty percent are referred to hospital care, mainly due to renal failure, poor glycaemic control and for a retinopathy assessment. Only 52% of those surveyed conducted medication reconciliation in the transition between healthcare levels. Fifty-eight percent reported conducting interconsultations, clinical meetings or consultancies between healthcare levels. The 3 main factors identified for improving the follow-up and control of DM2 with comorbidity were the multidisciplinary study (80.8%), the continuing education of health professionals (72.3%) and therapeutic education programs (72%). A lack of time, a lack of qualified personnel for lifestyle interventions and organizational shortcomings were mentioned as the main obstacles for improving the care of these patients.
ConclusionsMost patients with DM2 and comorbidity are treated in Primary Care. Promoting multidisciplinary care and training programs for practitioners and patients can help improve the quality of care. Therapy reconciliation represents a priority area for improvement in this population.
Analizar la atención que reciben los pacientes con diabetes mellitus tipo 2 (DM2) y comorbilidad en el Sistema Nacional de Salud español.
Pacientes y métodosEstudio transversal mediante encuesta online. Participaron 302 médicos de familia, internistas y endocrinólogos, reclutados por sus respectivas sociedades científicas, de manera voluntaria y no retribuida.
ResultadosLos pacientes con DM2 y comorbilidad son atendidos mayoritariamente en Atención Primaria (71,8%). Un 40% son derivados a atención hospitalaria, principalmente por insuficiencia renal, mal control glucémico y evaluación de retinopatía. Solo el 52% de los encuestados realizaban conciliación farmacológica en la transición entre niveles asistenciales. El 58% manifestaron realizar interconsultas, sesiones clínicas o consultorías entre niveles asistenciales. Los 3 principales factores identificados para mejorar el seguimiento y control de la DM2 con comorbilidad fueron el trabajo multidisciplinar (80,8%), la formación continuada de los profesionales sanitarios (72,3%) y los programas de educación terapéutica (72%). La falta de tiempo, la carencia de personal cualificado en intervenciones sobre el estilo de vida y las deficiencias organizativas fueron citadas como las principales barreras para la mejora asistencial en estos pacientes.
ConclusionesLa mayoría de los pacientes con DM2 y comorbilidad son atendidos en Atención Primaria. Promover la atención multidisciplinaria y los programas formativos para profesionales y pacientes puede contribuir a mejorar la calidad asistencial. La conciliación terapéutica representa un área prioritaria de mejora en esta población.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<