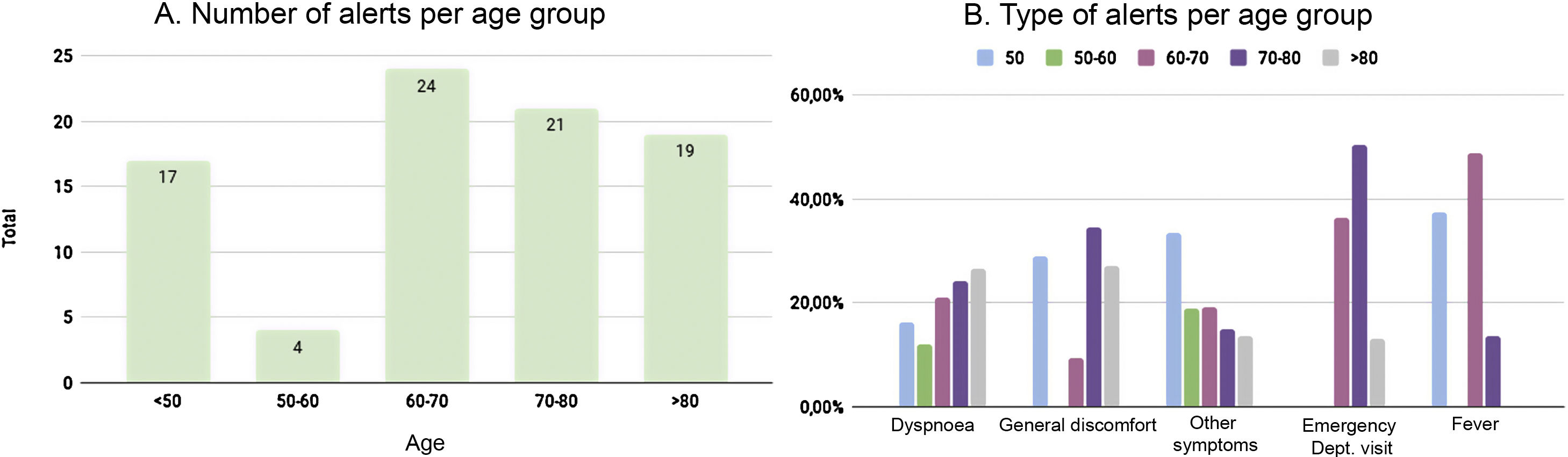
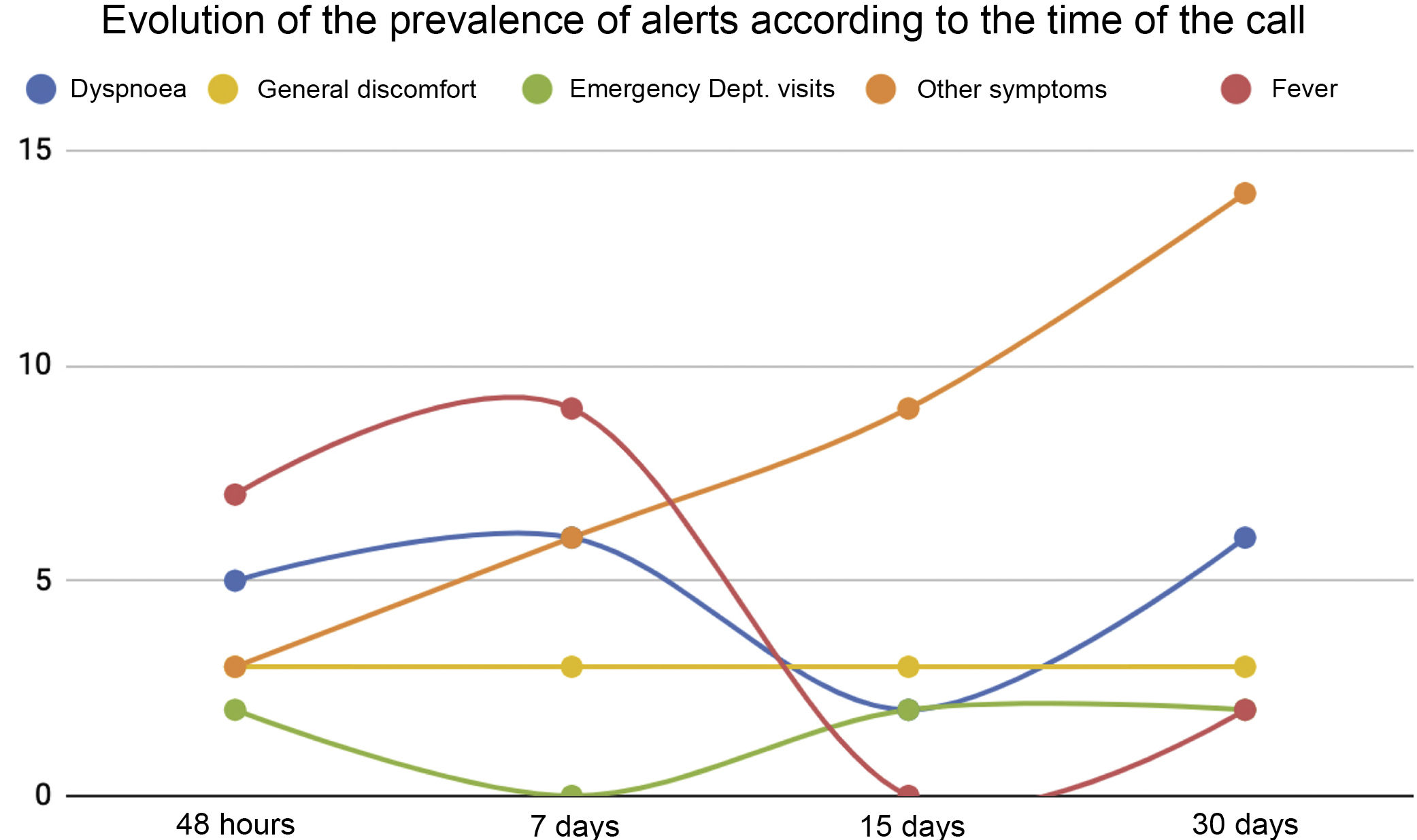
COVID-19 has placed a significant burden on the healthcare system, making it necessary to implement new tools that allow patients to be monitored remotely and guarantee quality and continuity of care. The usefulness and acceptance by patients of a virtual caregiver designed for follow-up in the month following hospital discharge for COVID-19 are evaluated. The virtual assistant, based on voice and artificial intelligence technology, made telephone calls at 48 h, seven days, 15 days, and 30 days after discharge and asked five questions about the patient’s health. If the answer to any of the questions was affirmative, it generated an alert that was transferred to a healthcare professional One hundred patients were included in the project and 85 alerts were generated in 45 of the patients, most at one month after hospital discharge. The nursing staff resolved 94% of them by telephone. Patient satisfaction with the virtual caregiver was high.
La COVID-19 ha supuesto una gran sobrecarga para el sistema sanitario, y ha sido necesario poner en marcha herramientas nuevas para realizar el seguimiento no presencial de los pacientes y garantizar la calidad de sus cuidados. Se evalúa la utilidad y aceptación de los pacientes de un cuidador virtual diseñado para su seguimiento tras el alta hospitalaria por COVID-19. El asistente virtual, con tecnología de voz e inteligencia artificial, realizó llamadas telefónicas a las 48 horas, 7, 15 y 30 días del alta, formulando 5 preguntas sobre su estado de salud. Si la contestación era afirmativa, generaba una alerta que se transfería a un profesional sanitario. Se incluyeron 100 pacientes en el proyecto. Se generaron 85 alertas en 45 de los pacientes, la mayoría de ellas al mes del alta; el 94% lo resolvió enfermería telefónicamente. La satisfacción de los pacientes con el cuidador virtual fue alta.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<