The performance of invasive procedures in patients undergoing oral anticoagulation represents a risk. Without conclusive data on this issue, the recommendations on managing oral anticoagulation are generally weak, and its management is controversial and heterogeneous.
We conducted a review of the evidence on the elective periprocedural management of oral anticoagulation following the publication of the 9th edition of the guidelines of the American College of Chest Physicians.
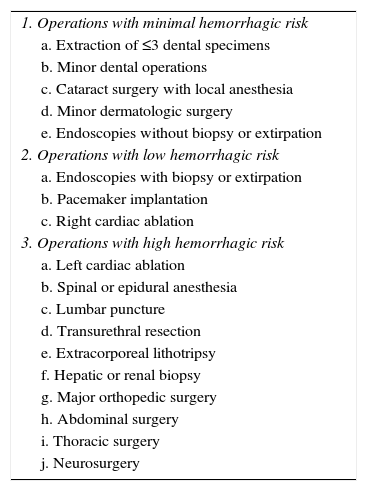
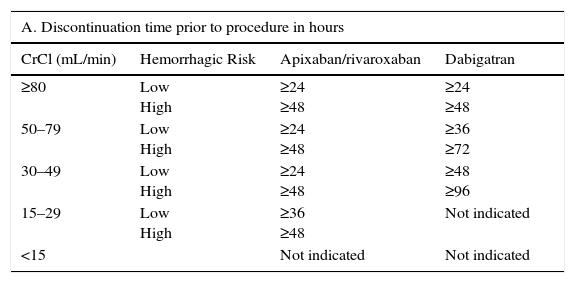
Except for cases of procedures with minimal hemorrhagic risk, the use of oral anticoagulants is suspended with sufficient time so that it can be performed without a significant anticoagulant effect, which will depend on the half-life of the drug. For direct oral anticoagulants, the half-life is determined by the renal function.
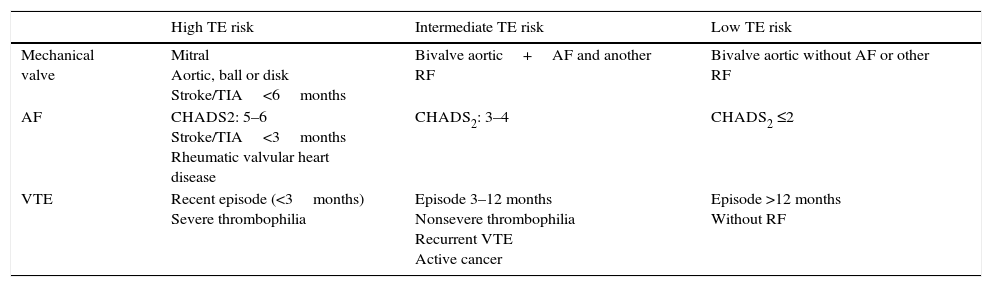
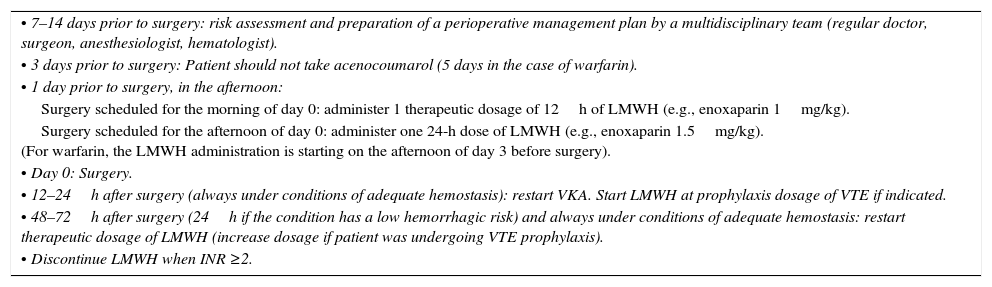
Recent studies have shown that the use of bridge therapy with heparin in patients who temporarily suspended the use of oral anticoagulation provided no benefits and increased the bleeding. However, there is no conclusive evidence against its use in patients with a high thromboembolic risk.
La realización de procedimientos invasivos en pacientes con anticoagulación oral es un riesgo. Sin unos datos concluyentes al respecto, las recomendaciones sobre el manejo, por lo general, son de escasa solidez, y su manejo es controvertido y heterogéneo.
Se realiza una revisión de las evidencias sobre el manejo periprocedimiento electivo de la anticoagulación oral después de la publicación de la 9.ª edición de la guía del American College of Chest Physicians.
Salvo en caso de procedimientos con riesgo hemorrágico mínimo, los anticoagulantes orales serán suspendidos justo con la antelación necesaria para que se realice sin efecto anticoagulante significativo, lo que dependerá de la vida media del fármaco, que en el caso de los anticoagulantes orales de acción directa está condicionada por la función renal.
Estudios recientes muestran que la utilización de terapia puente con heparina en pacientes que interrumpen temporalmente la anticoagulación oral no aporta beneficios e incrementa los sangrados; sin embargo, no hay evidencia concluyente contra su uso en pacientes con alto riesgo tromboembólico.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<