Despite the increasing evidence supporting the importance of airborne transmission in SARS-CoV-2 infection, it has not been considered relevant in the vast majority of reported nosocomial outbreaks of COVID-19. The aim of this study is to describe a nosocomial outbreak of SARS-CoV-2 infection whose features suggest that aerosol transmission had an important role.
MethodsThis is a descriptive analysis of a nosocomial outbreak of SARS-CoV-2 infection in an internal medicine ward that occurred in December 2020. All cases were confirmed by a positive PCR test for SARS-CoV-2.
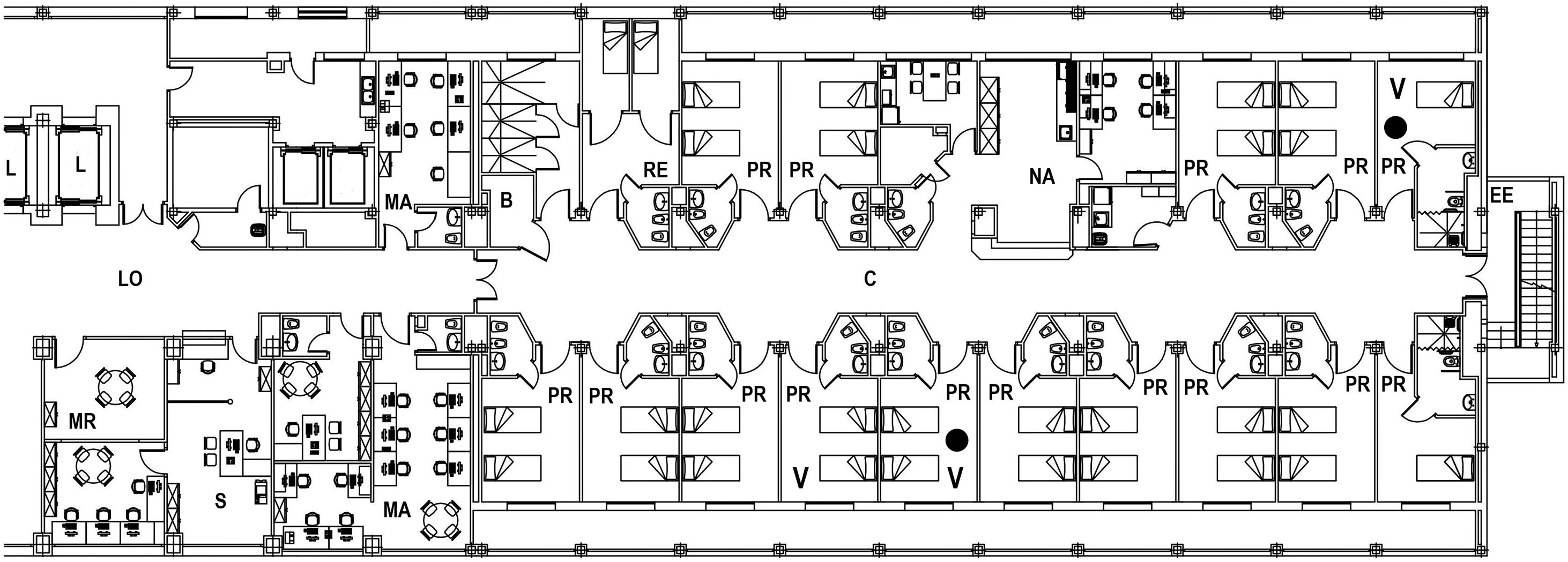
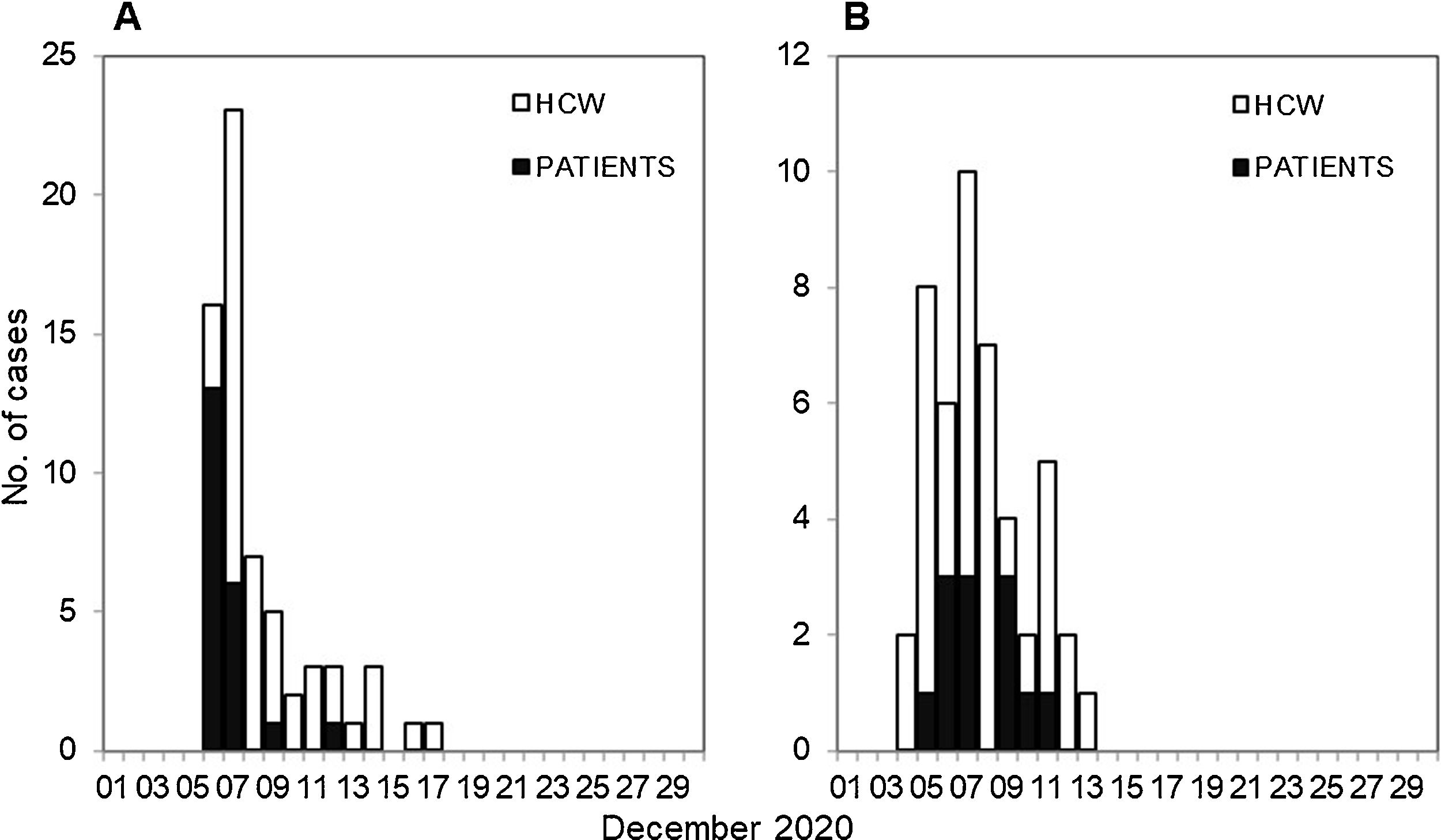
ResultsFrom December 5 to December 17, 21 patients and 44 healthcare workers (HCWs) developed a nosocomial SARS-CoV-2 infection. Fifty-one of the 65 cases (78.5%) were diagnosed between December 6 and 9. The attack rate in patients was 80.8%. Among HCWs, the attack rate was higher in those who had worked at least one full working day in the ward (56.3%) than in those who had occasionally been in the ward (25.8%; p = 0.005). Three days before the first positive case was detected, two extractor fans were found to be defective, affecting the ventilation of three rooms. Sixteen cases were asymptomatic, 48 cases had non-severe symptoms, and 2 cases required admission to the intensive care unit. All patients eventually recovered.
ConclusionThe high attack rate, the explosive nature of the outbreak, and the coincidence in time with the breakdown in air extractors in some rooms of the ward suggest that airborne transmission played a key role in the development of the outbreak.
A pesar de los datos cada vez mayores que respaldan la importancia de la transmisión aérea en la infección por el SARS-CoV-2, en la inmensa mayoría de los brotes nosocomiales descritos de COVID-19 no se ha considerado relevante. El objetivo de este estudio consiste en describir un brote nosocomial de infección por el SARS-CoV-2 cuyas características indican que la transmisión por aerosoles desempeñó un papel importante.
MétodosSe trata de un análisis descriptivo de un brote nosocomial de infección por el SARS-CoV-2 en una planta de Medicina Interna que tuvo lugar en diciembre de 2020. Todos los casos se confirmaron mediante una PCR positiva para SARS-CoV-2.
ResultadosEntre el 5 y el 17 de diciembre, 21 pacientes y 44 profesionales sanitarios contrajeron una infección nosocomial por el SARS-CoV-2. De los 65 casos, 51 (78,5%) se diagnosticaron entre el 6 y el 9 de diciembre. La tasa de ataque en los pacientes fue del 80,8%. Entre los profesionales sanitarios, la tasa de ataque fue mayor en los que habían trabajado al menos una jornada laboral completa en la planta (56,3%) que en los que habían estado ocasionalmente en ella (25,8%; p = 0,005). Tres días antes de detectar el primer caso positivo se identificó una avería en dos extractores de aire, que afectó a la ventilación de tres habitaciones. Dieciséis casos cursaron de forma asintomática, 48 manifestaron síntomas leves y 2 precisaron ingreso en la unidad de cuidados intensivos. Todos los casos se recuperaron finalmente.
ConclusionesLa elevada tasa de ataque, la naturaleza explosiva del brote y la coincidencia en el tiempo con la avería de los extractores de aire en algunas habitaciones de la planta indican que la transmisión aérea desempeñó un papel fundamental en el desarrollo del brote.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<