To evaluate the independent usefulness of pleural fluid smear and cell block (CB) preparations for the diagnosis of malignant effusions.
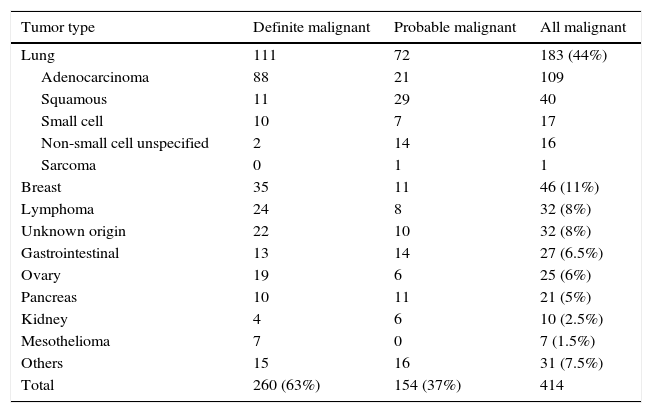
Patients and methodsA total of 632 cytological smears and 554 CBs from 414 consecutive patients with malignant effusions were retrospectively evaluated.
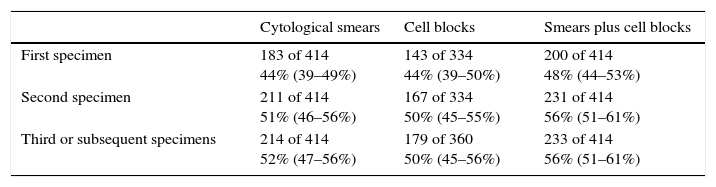
ResultsThe diagnostic yield of a first specimen was 44% regardless of whether a smear or CB cytologic examination was performed. The use of subsequent separated specimens increased the identification of malignancy to 56%. Overall, 11% of samples found to be negative by cytologic smears showed malignant cells on CBs, whereas 15% of negative CBs were reported as positive on smear slides. Pleural fluid specimens with low red and/or white blood cell counts more frequently resulted in the generation of suboptimal CB preparations.
ConclusionsIf CBs and smears are prepared and examined, the percentage of positive diagnoses will be greater than if only one method is used.
Evaluar la utilidad independiente de frotis y bloques celulares (BC) del líquido pleural para diagnosticar derrames malignos.
Pacientes y métodosSe evaluaron retrospectivamente un total de 632 frotis citológicos y 554 BC de 414 pacientes consecutivos con derrame pleural maligno.
ResultadosLa sensibilidad diagnóstica de una primera muestra fue del 44%, tanto en frotis como en BC. El análisis de muestras separadas ulteriores aumentó al 56% la identificación de derrames malignos. Globalmente, el 11% de muestras negativas mediante frotis mostraron células malignas en los BC, mientras que el 15% de BC negativos resultaron positivos en el estudio del frotis. Los líquidos pleurales con recuentos bajos de hematíes o leucocitos produjeron con mayor frecuencia BC insuficientes para diagnóstico.
ConclusionesSi se evalúan frotis y BC, el porcentaje de resultados positivos es superior que si se emplean estas técnicas de forma aislada.
Artículo
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<