This work aimed to compare the characteristics, progress, and prognosis of patients with COPD hospitalized due to COVID-19 in Spain in the first wave with those of the second wave.
Material and methodsThis is an observational study of patients hospitalized in Spain with a diagnosis of COPD included in the SEMI-COVID-19 registry. The medical history, symptoms, analytical and radiological results, treatment, and progress of patients with COPD hospitalized in the first wave (from March to June 2020) versus those hospitalized in the second wave (from July to December 2020) were compared. Factors associated with poor prognosis, defined as all-cause mortality and a composite endpoint that included mortality, high-flow oxygen therapy, mechanical ventilation, and ICU admission, were analyzed.
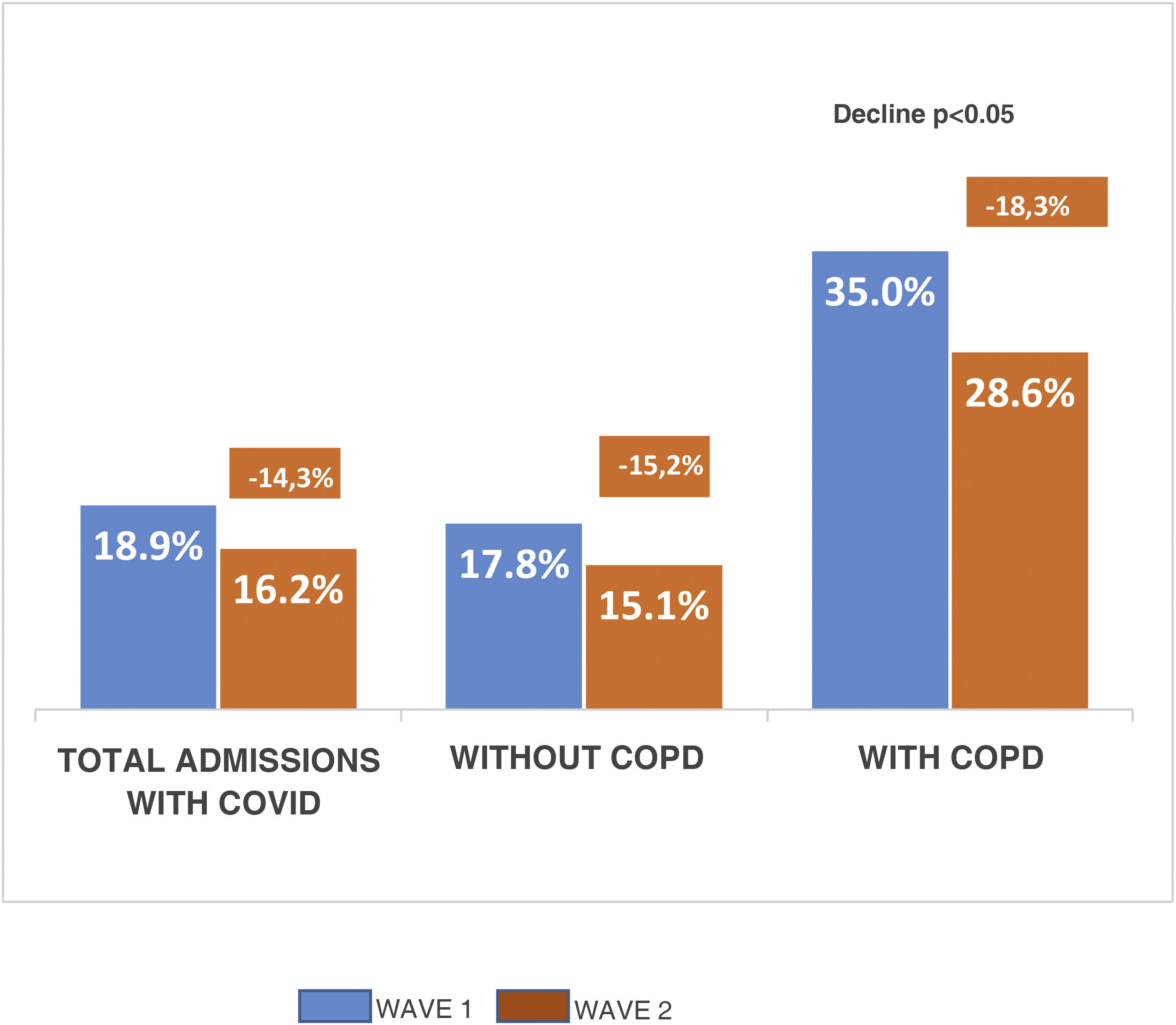
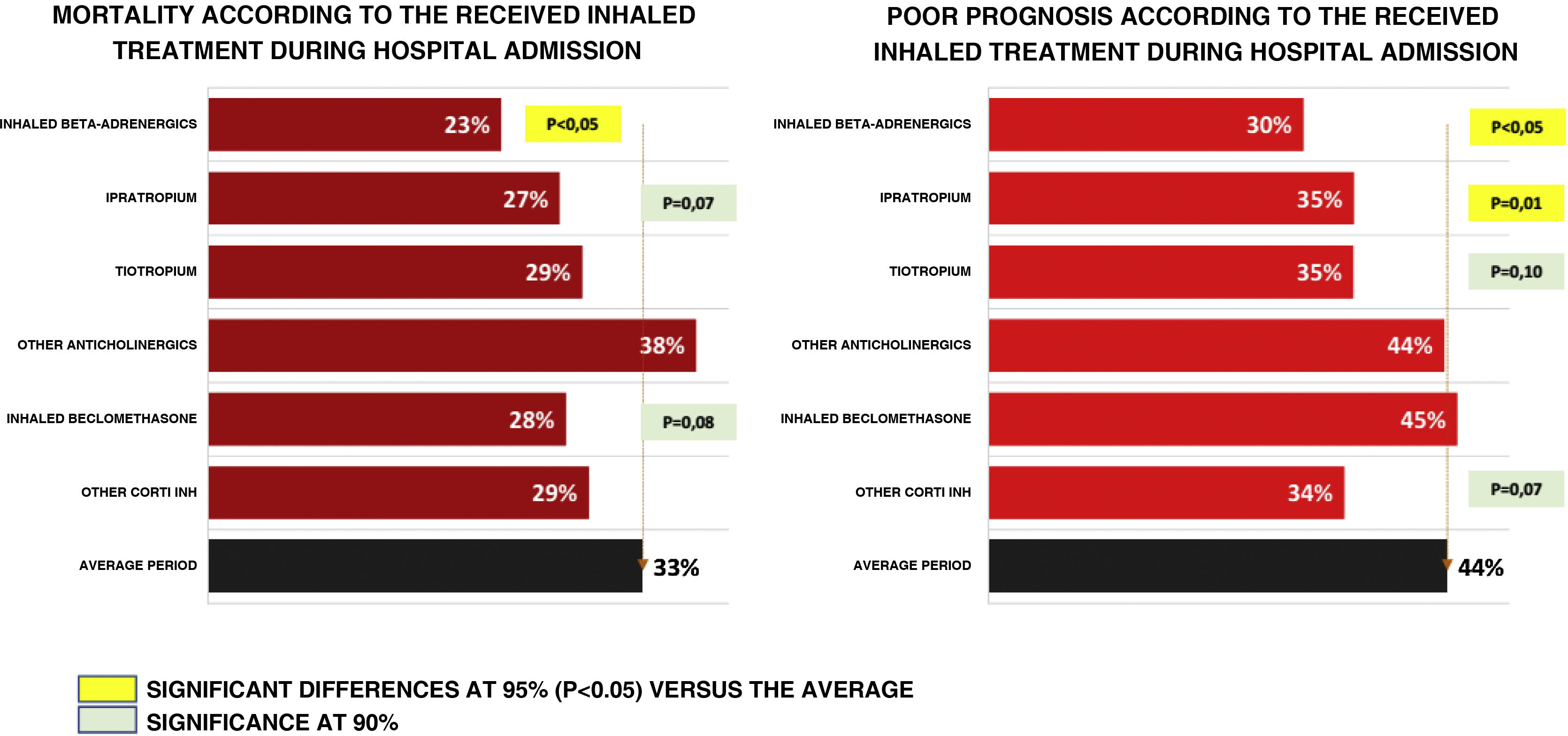
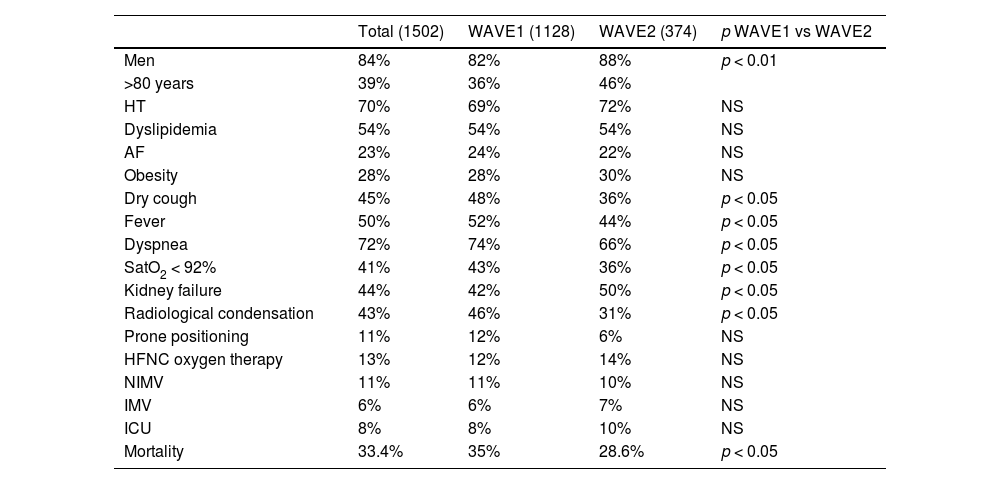
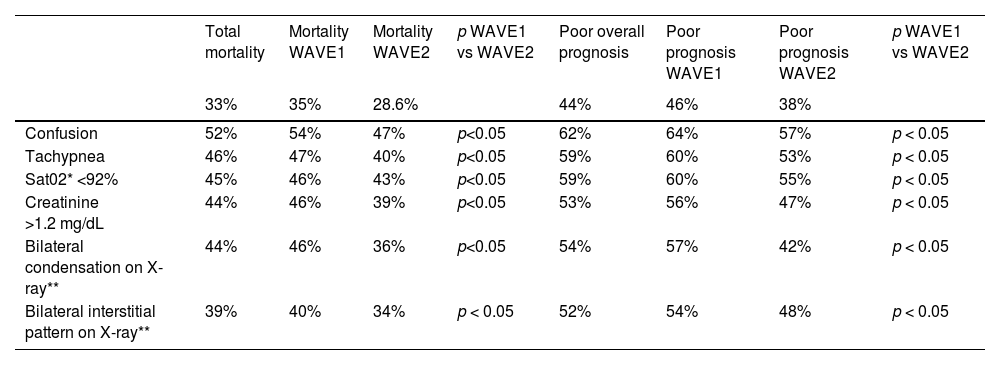
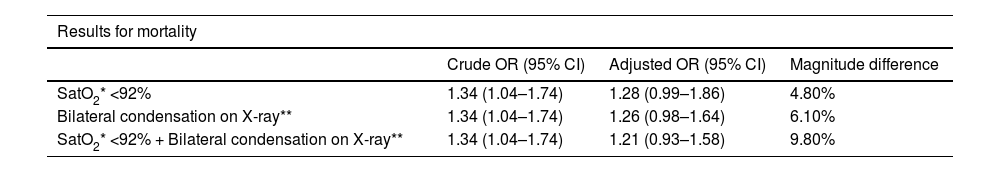
ResultsOf the 21,642 patients in the SEMI-COVID-19 Registry, 6.9% were diagnosed with COPD: 1128 (6.8%) in WAVE1 and 374 (7.7%) in WAVE2 (p = 0.04). WAVE2 patients presented less dry cough, fever and dyspnea, hypoxemia (43% vs 36%, p < 0.05), and radiological condensation (46% vs 31%, p < 0.05) than WAVE1 patients. Mortality was lower in WAVE2 (35% vs 28.6%, p = 0.01). In the total sample, mortality and the composite outcome of poor prognosis were lower among patients who received inhalation therapy.
ConclusionsPatients with COPD admitted to the hospital due to COVID-19 in the second wave had less respiratory failure and less radiological involvement as well as a better prognosis. These patients should receive bronchodilator treatment if there is no contraindication for it.
Comparar las características, evolución y pronóstico de los pacientes con EPOC hospitalizados por COVID-19 en España en la primera ola con los de la segunda ola.
Material y métodosEstudio observacional de los pacientes hospitalizados en territorio español con diagnóstico de EPOC incluidos en el registro SEMI-COVID-19.
Se compararon los antecedentes, la clínica, resultados analíticos y radiológicos, tratamiento y evolución de los pacientes con EPOC hospitalizados en la primera ola (desde marzo hasta junio 2020) frente a los hospitalizados en la segunda ola (desde julio hasta diciembre 2020). Se analizaron los factores de mal pronóstico, definidos como mortalidad por todas las causas y un evento combinado que incluía mortalidad, oxigenoterapia con alto flujo, ventilación mecánica e ingreso en UCI.
ResultadosDe 21,642 pacientes del Registro SEMI COVID-19, están diagnosticados de EPOC el 6,9%, 1128 (6,8%) en la OLA1 y 374 (7,7%) en la OLA2 (p = 0,04). Los pacientes de la OLA2 presentan menos tos seca, fiebre y disnea, hipoxemia (43% vs 36%, p < 0,05) y condensación radiológica (46% vs 31%, p < 0,05) que los de la OLA1. La mortalidad es menor en la OLA2 (35% vs 28,6%, p = 0,01). En el global de pacientes la mortalidad y la variable combinada de mal pronóstico fue menor entre los pacientes que recibieron tratamiento inhalador.
ConclusionesLos pacientes con EPOC con ingreso hospitalario por COVID-19 en la segunda ola presentan menos insuficiencia respiratoria y menos afectación radiológica, con mejor pronóstico. Estos pacientes deben recibir tratamiento broncodilatador si no hay contraindicación para el mismo.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<