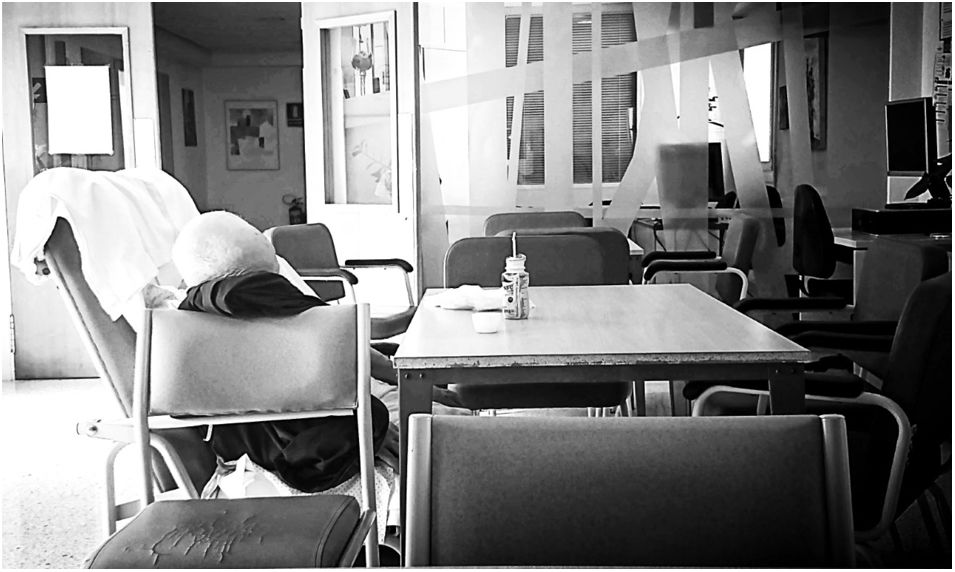
The rapid spread of SARS-CoV-2 requires evidence to help mitigate its global harm. Generating accurate measurements of the appropriate clinical and epidemiological indicators associated with COVID-19 is a necessary step in reducing the current pandemic's burden on individuals and the population at large. These unprecedented times have presented a challenge to chronic desease epidemiologists and have required a practical approach “to do something to help during this disaster”. Options include returning to clinical care or resorting to online textbooks and resources for crash courses on outbreak research. However, being aware of the magnitude of individual suffering endured by so many, including many esteemed and close colleagues, becomes a personal challenge of enormous proportions. It is envisaged that the arts and other humanities can help re-establish balance, both during the pandemic and especially after it.
La rápida propagación del SARS-CoV-2 requiere la generación de evidencia para ayudar a mitigar su daño global. La medición precisa con los indicadores clínicos y epidemiológicos apropiados asociados con COVID-19 es un paso necesario para reducir la carga individual y poblacional de la pandemia en curso. Estos tiempos sin precedentes han planteado un desafío para los epidemiólogos de enfermedades crónicas, y requirió de un enfoque práctico «para hacer algo para ayudar durante este desastre». Las opciones incluían regresar a la clínica asistencial o recurrir a libros de texto y recursos en línea para un curso acelerado sobre investigación de brotes. Sin embargo, ser consciente de la magnitud del sufrimiento individual soportado por tantos, incluyendo muchos colegas estimados y cercanos, se erige como un desafío personal de enormes proporciones. Se prevé que las artes y otras formas de Humanidades pueden ayudar a restablecer el equilibrio, tanto durante la pandemia, como especialmente después.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<