On January 7th, 2020, a new coronavirus, SARS-CoV-2, was identified, as responsible for a new human disease: COVID-19. Given its recent appearance, our current knowledge about the possible influence that this disease can exert on pregnancy is very limited. One of the unknowns to be solved is whether there is a vertical transmission of the infection during pregnancy.
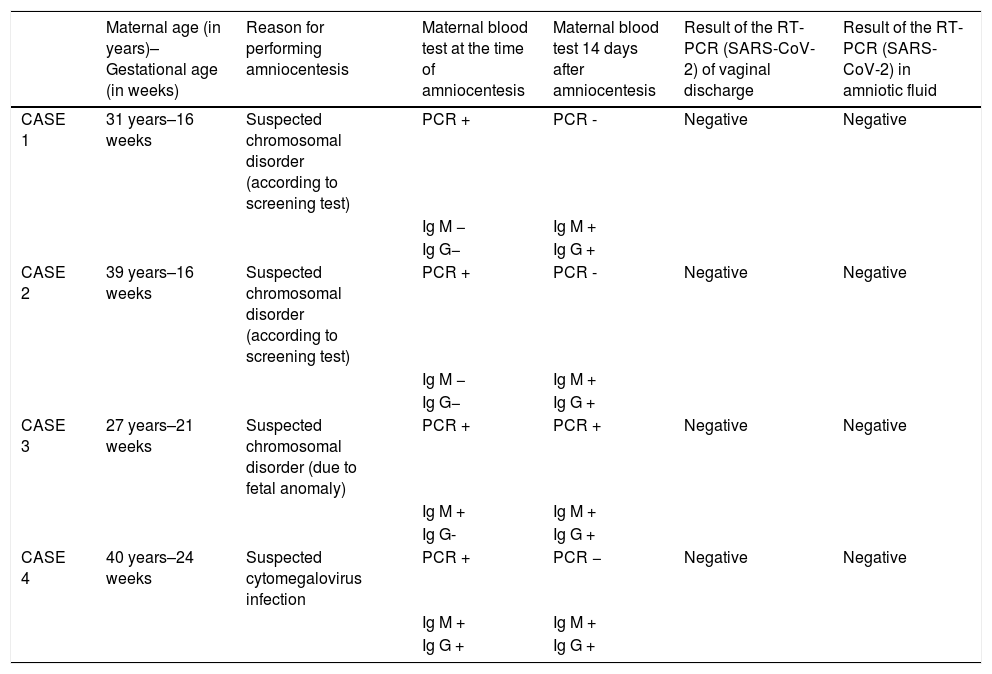
Patients and methodsUsing the Real-time Polymerase Chain Reaction techniques for SARS-CoV-2 nucleic acids, the possible presence of this germ in vaginal discharge and amniotic fluid was investigated in four pregnant Caucasian patients affected by mild acute symptoms of COVID-19 during the second trimester of pregnancy.
ResultsThere is no laboratory evidence to suggest a possible passage of SARS-CoV-2 from the infected mother to the amniotic fluid.
ConclusionsIt is necessary to expand the investigation of COVID-19 cases diagnosed during pregnancy to clarify the real influence that SARS-CoV-2 has on pregnant women and their offspring, as well as those factors that modulate the disease.
El pasado 7 de enero de 2020 se identificó un nuevo coronavirus, el SARS-CoV-2, responsable de una nueva enfermedad en el humano: la COVID-19. Dada su reciente aparición, nuestro conocimiento actual sobre la posible influencia que esta enfermedad puede ejercer en el embarazo es muy limitado. Una de las incógnitas que hay que despejar es si existe transmisión vertical de la infección durante la gestación.
Pacientes y métodosMediante técnicas de reacción en cadena de la polimerasa en tiempo real para ácidos nucleicos del SARS-CoV-2 se investigó la posible presencia de dicho germen en el flujo vaginal y el líquido amniótico de cuatro pacientes embarazadas de raza caucásica afectadas por cuadros agudos leves de COVID-19 durante el segundo trimestre de la gestación.
ResultadosNo existen evidencias de laboratorio que sugieran un posible paso del SARS-CoV-2 desde la madre infectada al líquido amniótico.
ConclusionesEs preciso ampliar la investigación de casos de COVID-19 diagnosticados durante la gestación para poder aclarar la influencia real que el SARS-CoV-2 ejerce sobre las embarazadas y su descendencia, así como aquellos factores que modulan la enfermedad.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<