1890 - EVOLUCIÓN CLÍNICA, ANALÍTICA Y RADIOLÓGICA DE LOS PACIENTES INGRESADOS POR SARS-COV-2 A LOS 3 MESES DEL ALTA HOSPITALARIA
Hospital de Mataró (Consorci Sanitari del Maresme), Mataró, España.
Objetivos: Analizar la evolución clínica, analítica y radiológica a los 3 meses del ingreso hospitalario por infección por SARS-CoV-2 en pacientes no inmunizados previamente contra el COVID-19, según el tratamiento administrado.
Métodos: Estudio de cohortes unicéntrico, obteniendo información entre junio 2020 y enero 2021 de los supervivientes ingresados por infección por SARS-CoV-2 que acuden a la visita de seguimiento a los 3 meses desde el alta hospitalaria. Se incluyeron los pacientes que cumplían los criterios y otorgaron su consentimiento verbal, registrado en su historia clínica. El estudio fue aprobado por el comité ético de investigación clínica de nuestro centro. La recogida de datos se realizó retrospectivamente, obteniendo datos clínicos, radiológicos, analíticos y terapéuticos previos, durante y posteriores al ingreso.
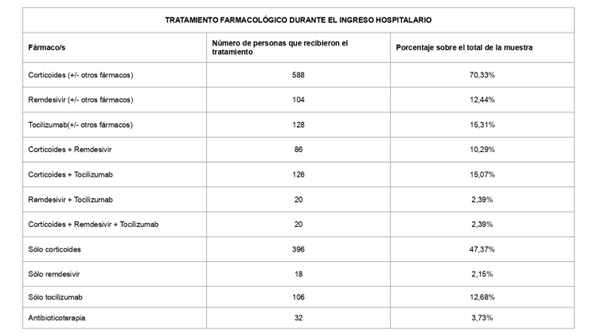
Resultados: Se han obtenido resultados de 858 pacientes. La media de edad muestral es de 60,26 años [20-94 años], siendo el 39,81% mujeres y el 60,19%, hombres. El 6,60% es personal sanitario. El 47,67% refería conocer exposición a SARS-CoV-2 previa a su infección. Durante el ingreso, los pacientes recibieron tratamiento farmacológico con corticoides (70,33%), remdesivir (12,44%) y tocilizumab (15,31%). Del total, se asociaron dexametasona y remdesivir en el 10,29%, dexametasona y tocilizumab en el 15,07%, remdesivir y dexametasona en el 2,39% y los tres fármacos en el 2,39%. Fueron visitados a los 102 días de promedio desde el alta, refiriendo un estado de salud subjetivo de 4,18 puntos [1-5]. La sintomatología persistente más frecuente fue la astenia (41,26%) y la disnea (30,89%). Otros síntomas fueron alopecia (15,03%), alteraciones sensitivas (14,8%), artromialgias (14,69%), cefalea (10,72%), anosmia (10,02%), alteraciones visuales (8,74%), disgeneusia (8,74%), tos seca (8,04%), anorexia (6,29%), odinofagia (5,24%), tos con expectoración (2,91%), diarreas (2,56%), dolor abdominal (1,98%) y náuseas (0,70%). Un 43,36% refería pérdida de peso (con promedio de 3,26 Kg) y un 0,58%, fiebre persistente. Los pacientes que recibieron corticoides presentaron astenia y disnea persistente en el 2,79% y 21,79%, respectivamente. En el caso de remdesivir fueron el 0,93% y 4,90%, y con tocilizumab 1,05% y 6,18%. La sintomatología secundaria mejoró en un 60% en aquellos que recibieron corticoides, remdesivir y/o tocilizumab. Hubo mejoría radiológica en el 94,27% del total, aunque en el 7,99% persistía un infiltrado intersticial y en el 1,73% consolidación. Se vio una mejoría radiológica por usar corticoides en 4 pacientes y remdesivir en 2. Analíticamente, mostraban 1,01 g/dL de gammaglobulinas de media [valores normales 0,8-1,4 g/dL] y 2.194,32 linfocitos/μL [valores normales: 4.000-10.000] y en el 98,60% se observaron anticuerpos antinucleocápside para SARS-CoV-2 positivos. Del total de 630 pacientes que recibieron algún tratamiento específico, el 12,70% presentaban hipogammaglobulinemia y el 73,20% linfopenia. De los que solo recibieron tratamiento sintomático, el 10,96% tenía hipogammaglobulinemia y el 26,80% linfopenia.
Conclusiones: Los pacientes que recibieron algún tratamiento específico mostraron una clara mejoría clínica. Puede existir una relación entre su uso y linfopenia, sin evidenciarse cambios considerables en los niveles de gammaglobulinas. No hay grandes diferencias radiológicas según el tratamiento usado en este estudio. El mayor impacto terapéutico consiste en la mejoría sintomática, que no siempre va acompañado de una mejora analítica y radiológica proporcional.
Bibliografía
- Sharma A, Ahmad Farouk I, Lal SK. COVID-19: A Review on the Novel Coronavirus Disease Evolution, Transmission, Detection, Control and Prevention. Viruses. 2021 Jan 29;13(2):202.
- Chavda VP, Vuppu S, Mishra T, et al. Recent review of COVID-19 management: diagnosis, treatment and vaccination. Pharmacol Rep. 2022 Dec;74(6):1120-48.
- Winkler MS, Osuchowski MF, Payen D, et al. Renaissance of glucocorticoids in critical care in the era of COVID-19: ten urging questions. Crit Care. 2022;26(1):308.
- Registro SEMI-COVID-19. Sociedad Española de Medicina Interna. 2019 - at present. https://www.fesemi.org/investigacion/proyectos/registro-semi-covid-19
- COVIDCAT Research. Covid-19 cohort in Catalonia. ISGlobal. https://www.isglobal.org/en/-/covicat
- Castanares-Zapatero D, Chalon P, Kohn L, et al. Pathophysiology and mechanism of long COVID: a comprehensive review. Ann Med. 2022 Dec;54(1):1473-87.
- Batiha GE, Al-Kuraishy HM, Al-Gareeb AI, et al. Pathophysiology of Pos-COVID syndromes: a new perspective. Virol J. 2022;19(1):158.
- Moreno-Pérez O, Merino E, Leon-Ramírez JM, et al; COVID-19-ALC research group. Post-acute COVID-19 syndrome. Incidence and risk factors: A Mediterranean cohort study. J Infect. 2021;82(3):378-83.
- Peramo-Álvarez FP, López-Zúñiga MÁ, López-Ruz MÁ. Medical sequels of COVID-19. Med Clin (Barc). 2021;157(8):388-94.
- López-Sampalo A, Bernal-López MR, Gómez-Huelgas R. Persistent COVID-19 syndrome. A narrative review. Rev Clin Esp (Barc). 2022 Apr;222(4):241-50.
- Pierce JD, Shen Q, Cintron SA, et al. Pos-COVID-19 Syndrome. Nurs Res. 2022 Mar-Apr 01;71(2):164-74.
- Thurnher MM, Reith W, Thurnher AP, Rommer P. Long-COVID: Langzeitsymptome und morphologische/radiologische Korrelate [Long COVID: long-term symptoms and morphological/radiological correlates]. Radiologe. 2021 Oct;61(10):915-22.
- Bungenberg J, Humkamp K, Hohenfeld C, et al. Long COVID-19: Objectifying most self-reported neurological symptoms. Ann Clin Transl Neurol. 2022 Feb;9(2):141-54.
- Naeije R, Caravita S. Phenotyping long COVID. Eur Respir J. 2021 Aug 26;58(2):2101763.
- Duggal P, Penson T, Manley HN, et al. Post-sequelae symptoms and comorbidities after COVID-19. J Med Virol. 2022 May;94(5):2060-6.
- Moghimi N, Di Napoli M, Biller J, et al. The Neurological Manifestations of Post-Acute Sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021 Jun 28;21(9):44.
- Tana C, Bentivegna E, Cho SJ, et al. Long COVID headache. J Headache Pain. 2022 Aug 1;23(1):93.
- Tleyjeh IM, Kashour T, Riaz M, et al. Persistent COVID-19 symptoms at least one month after diagnosis: A national survey. J Infect Public Health. 2022 May;15(5):578-85.
- Tosato M, Carfì A, Martis I, et al; Gemelli Against COVID-19 Post-Acute Care Team. Prevalence and Predictors of Persistence of COVID-19 Symptoms in Older Adults: A Single-Center Study. J Am Med Dir Assoc. 2021 Sep;22(9):1840-4.
- Hossain MA, Hossain KMA, Saunders K, et al. Prevalence of Long COVID symptoms in Bangladesh: a prospective Inception Cohort Study of COVID-19 survivors. BMJ Glob Health. 2021 Dec;6(12):e006838.
- Ramadan MS, Bertolino L, Zampino R, et al.; Monaldi Hospital Cardiovascular Infection Study Group. Cardiac sequelae after coronavirus disease 2019 recovery: a systematic review. Clin Microbiol Infect. 2021 Sep;27(9):1250-1261.
- Daines L, Zheng B, Pfeffer P, et al.. A clinical review of long-COVID with a focus on the respiratory system. Curr Opin Pulm Med. 2022 May 1;28(3):174-9.
- Peghin M, De Martino M, Palese A, et al. Pos-COVID-19 syndrome and humoral response association after 1 year in vaccinated and unvaccinated patients. Clin Microbiol Infect. 2022 Aug;28(8):1140-8.
- Alghamdi HY, Alrashed AM, Jawhari AM, et al. Neuropsychiatric symptoms in pos-COVID-19 long haulers. Acta Neuropsychiatr. 2022 Dec;34(6):318-29.
- Van Herck M, Goërtz YMJ, Houben-Wilke S, et al. Severe Fatigue in Long COVID: Web-Based Quantitative Follow-up Study in Members of Online Long COVID Support Groups. J Med Internet Res. 2021 Sep 21;23(9):e30274.
- Hennigs JK, Oqueka T, Harbaum L, et al. Organbezogene Folgeerscheinungen von COVID 19 bei Erwachsenen [Organ-specific sequelae of COVID-19 in adults]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2022 Apr;65(4):462-70.
- Robineau O, Zins M, Touvier M, et al; Santé, Pratiques, Relations et Inégalités Sociales en Population Générale Pendant la Crise COVID-19-Sérologie (SAPRIS-SERO) Study Group. Long-lasting Symptoms After an Acute COVID-19 Infection and Factors Associated With Their Resolution. JAMA Netw Open. 2022 Nov 1;5(11):e2240985.
- Carfì A, Bernabei R, Landi F; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020 Aug 11;324(6):603-5.
- Sykes DL, Holdsworth L, Jawad N, et al. Pos-COVID-19 Symptom Burden: What is Long-COVID and How Should We Manage It? Lung. 2021 Apr;199(2):113-9.
- Mandal S, Barnett J, Brill SE, et al. 'Long-COVID': a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax. 2021 Apr;76(4):396-8.
- Peghin M, Palese A, Venturini M, , et al. Pos-COVID-19 symptoms 6 months after acute infection among hospitalized and non-hospitalized patients. Clin Microbiol Infect. 2021 Oct;27(10):1507-13.
- Anaya JM, Rojas M, Salinas ML, et al. Pos-COVID syndrome. A case series and comprehensive review. Autoimmun Rev. 2021 Nov;20(11):102947.
- Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, et al. Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection. PLoS One. 2020 Dec 11;15(12):e0243882.
- Havervall S, Rosell A, Phillipson M, et al. Symptoms and Functional Impairment Assessed 8 Months After Mild COVID-19 Among Health Care Workers. JAMA. 2021 May 18;325(19):2015-6.
- Ghosn J, Piroth L, Epaulard O, et al.; French COVID cohort study and investigators groups. Persistent COVID-19 symptoms are highly prevalent 6 months after hospitalization: results from a large prospective cohort. Clin Microbiol Infect. 2021 Jul;27(7):1041.e1-1041.e4.
- Sneller MC, Liang CJ, Marques AR, et al. A Longitudinal Study of COVID-19 Sequelae and Immunity: Baseline Findings. Ann Intern Med. 2022 Jul;175(7):969-79.
- Ceban F, Ling S, Lui LMW, et al. Fatigue and cognitive impairment in Pos-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun. 2022 Mar;101:93-135.
- van Kessel SAM, Olde Hartman TC, Lucassen PLBJ, et al. Post-acute and long-COVID-19 symptoms in patients with mild diseases: a systematic review. Fam Pract. 2022 Jan 19;39(1):159-67.
- Nasserie T, Hittle M, Goodman SN. Assessment of the Frequency and Variety of Persistent Symptoms Among Patients With COVID-19: A Systematic Review. JAMA Netw Open. 2021 May 3;4(5):e2111417.
- Seeßle J, Waterboer T, Hippchen T, et al. Persistent Symptoms in Adult Patients 1 Year After Coronavirus Disease 2019 (COVID-19): A Prospective Cohort Study. Clin Infect Dis. 2022 Apr 9;74(7):1191-8.
- Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, et al. Defining Pos-COVID Symptoms (Post-Acute COVID, Long COVID, Persistent Pos-COVID): An Integrative Classification. Int J Environ Res Public Health. 2021 Mar 5;18(5):2621.
- Matta J, Wiernik E, Robineau O, et al.; Santé, Pratiques, Relations et Inégalités Sociales en Population Générale Pendant la Crise COVID-19-Sérologie (SAPRIS-SERO) Study Group. Association of Self-reported COVID-19 Infection and SARS-CoV-2 Serology Test Results With Persistent Physical Symptoms Among French Adults During the COVID-19 Pandemic. JAMA Intern Med. 2022 Jan 1;182(1):19-25.
- Mehandru S, Merad M. Pathological sequelae of long-haul COVID. Nat Immunol. 2022 Feb;23(2):194-202.
- Bell ML, Catalfamo CJ, Farland LV, et al. Post-acute sequelae of COVID-19 in a non-hospitalized cohort: Results from the Arizona CoVHORT. PLoS One. 2021 Aug 4;16(8):e0254347.
- Willi S, Lüthold R, Hunt A, et al. COVID-19 sequelae in adults aged less than 50 years: A systematic review. Travel Med Infect Dis. 2021 Mar-Apr;40:101995. doi:10.1016/j.tmaid.2021.101995.
- Kim Y, Bitna-Ha, Kim SW, et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect Dis. 2022 Jan 27;22(1):93.
- Søraas A, Kalleberg KT, Dahl JA, et al. Persisting symptoms three to eight months after non-hospitalized COVID-19, a prospective cohort study. PLoS One. 2021 Aug 26;16(8):e0256142.
- Förster C, Colombo MG, Wetzel AJ, et al. Persisting Symptoms After COVID-19. Dtsch Arztebl Int. 2022 Mar 11;119(10):167-74.
- Vollrath S, Bizjak DA, Zorn J, et al. Recovery of performance and persistent symptoms in athletes after COVID-19. PLoS One. 2022 Dec 7;17(12):e0277984.
- Desgranges F, Tadini E, Munting A, et al, the RegCOVID Research Group. Pos-COVID 19 Syndrome in Outpatients: a Cohort Study. J Gen Intern Med. 2022 Jun;37(8):1943-52.
- Bai F, Tomasoni D, Falcinella Cet al. Female gender is associated with long COVID syndrome: a prospective cohort study. Clin Microbiol Infect. 2022 Apr;28(4):611.e9-611.e16.
- Contreras PJ, Romero-Albino Z, Cuba-Fuentes MS. Description of frequent and persistent symptoms of COVID-19 among older adults who attend senior centers. Medwave. 2022 Jan 28;22(1):e8689.
- Perlis RH, Santillana M, Ognyanova K, et al. Prevalence and Correlates of Long COVID Symptoms Among US Adults. JAMA Netw Open. 2022 Oct 3;5(10):e2238804.
- D'Ascanio L, Pandolfini M, Cingolani C, et al. Olfactory Dysfunction in COVID-19 Patients: Prevalence and Prognosis for Recovering Sense of Smell. Otolaryngol Head Neck Surg. 2021 Jan;164(1):82-6.
- Fortini A, Torrigiani A, Sbaragli S, et al. COVID-19: persistence of symptoms and lung alterations after 3-6 months from hospital discharge. Infection. 2021 Oct;49(5):1007-15.
- Pérez-González A, Araújo-Ameijeiras A, Fernández-Villar A, et al.; Cohort COVID-19 of the Galicia Sur Health Research Institute. Long COVID in hospitalized and non-hospitalized patients in a large cohort in Northwest Spain, a prospective cohort study. Sci Rep. 2022 Mar 1;12(1):3369.
- Chopra N, Chowdhury M, Singh AK, et al. Clinical predictors of long COVID-19 and phenotypes of mild COVID-19 at a tertiary care centre in India. Drug Discov Ther. 2021;15(3):156-61.
- Tessitore E, Handgraaf S, Poncet A, et al. Symptoms and quality of life at 1-year follow up of patients discharged after an acute COVID-19 episode. Swiss Med Wkly. 2021 Dec 13;151:w30093.
- Seang S, Itani O, Monsel G, et al. Long COVID-19 symptoms: Clinical characteristics and recovery rate among non-severe outpatients over a six-month follow-up. Infect Dis Now. 2022 May;52(3):165-9.
- Ziauddeen N, Gurdasani D, O'Hara ME, et al. Characteristics and impact of Long Covid: Findings from an online survey. PLoS One. 2022 Mar 8;17(3):e0264331.
- Darley DR, Dore GJ, Cysique L, et al. Persistent symptoms up to four months after community and hospital-managed SARS-CoV-2 infection. Med J Aust. 2021 Apr;214(6):279-80.
- Varela-Tapia CL, Contreras-Del Carmen N, Hernández-Amaro H, et al. Sintomatología cardiorrespiratoria y neuromusculoesquelética en COVID-19 posagudo en una unidad de rehabilitación [Cardiorespiratory and neuromusculoskeletal symptoms with post-acute COVID-19 in a Rehabilitation center]. Rev Med Inst Mex Seguro Soc. 2022 Jul 4;60(4):395-401.
- Mantovani E, Mariotto S, Gabbiani D, et al. Chronic fatigue syndrome: an emerging sequela in COVID-19 survivors? J Neurovirol. 2021 Aug;27(4):631-7.
- Irisson-Mora I, Salgado-Cordero AM, Reyes-Varón E, et al; Occupational Health and Preventive Medicine Consortium. Comparison between the persistence of post COVID-19 symptoms on critical patients requiring invasive mechanical ventilation and non-critical patients. PLoS One. 2022 Aug 22;17(8):e0273041.
- Garrigues E, Janvier P, Kherabi Y, et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020 Dec;81(6):e4-e6.
- Hellmuth J, Barnett TA, Asken BM, et al. Persistent COVID-19-associated neurocognitive symptoms in non-hospitalized patients. J Neurovirol. 2021 Feb;27(1):191-5.
- López-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021 Aug 9;11(1):16144.
- Premraj L, Kannapadi NV, Briggs J, et al. Mid and long-term neurological and neuropsychiatric manifestations of pos-COVID-19 syndrome: A meta-analysis. J Neurol Sci. 2022 Mar 15;434:120162.
- Taribagil P, Creer D, Tahir H. 'Long COVID' syndrome. BMJ Case Rep. 2021 Apr 19;14(4):e241485. doi:10.1136/bcr-2020-241485.
- Dennis A, Wamil M, Alberts J, et al.; COVERSCAN study investigators. Multiorgan impairment in low-risk individuals with pos-COVID-19 syndrome: a prospective, community-based study. BMJ Open. 2021 Mar 30;11(3):e048391.
- Global Burden of Disease Long COVID Collaborators, Wulf Hanson S, Abbafati C, Aerts JG, et al. Estimated Global Proportions of Individuals With Persistent Fatigue, Cognitive, and Respiratory Symptom Clusters Following Symptomatic COVID-19 in 2020 and 2021. JAMA. 2022 Oct 25;328(16):1604-15.
- Romero-Duarte Á, Rivera-Izquierdo M, Guerrero-Fernández de Alba I, et al. Sequelae, persistent symptomatology and outcomes after COVID-19 hospitalization: the ANCOHVID multicentre 6-month follow-up study. BMC Med. 2021 May 20;19(1):129.
- Rosales-Castillo A, García de Los Ríos C, Mediavilla García JD. Persistent symptoms after acute COVID-19 infection: importance of follow-up. Med Clin (Barc). 2021 Jan 8;156(1):35-6.
- Mahmud R, Rahman MM, Rassel MA, et al. Pos-COVID-19 syndrome among symptomatic COVID-19 patients: A prospective cohort study in a tertiary care center of Bangladesh. PLoS One. 2021 Apr 8;16(4):e0249644.
- Fernández-de-Las-Peñas C, Guijarro C, Plaza-Canteli S, et al. Prevalence of Pos-COVID-19 Cough One Year After SARS-CoV-2 Infection: A Multicenter Study. Lung. 2021 Jun;199(3):249-53.
- Agergaard J, Leth S, Pedersen TH, et al. Myopathic changes in patients with long-term fatigue after COVID-19. Clin Neurophysiol. 2021 Aug;132(8):1974-81.
- Aranda J, Oriol I, Feria L, et al. Persistent COVID-19 symptoms 1 year after hospital discharge: A prospective multicenter study. PLoS One. 2022 Oct 10;17(10):e0275615.
- Kingery JR, Safford MM, Martin P, et al. Health Status, Persistent Symptoms, and Effort Intolerance One Year After Acute COVID-19 Infection. J Gen Intern Med. 2022 Apr;37(5):1218-25.
- Rivera-Izquierdo M, Láinez-Ramos-Bossini AJ, de Alba IG, et al. Long COVID 12 months after discharge: persistent symptoms in patients hospitalised due to COVID-19 and patients hospitalised due to other causes-a multicentre cohort study. BMC Med. 2022 Feb 23;20(1):92.
- Naik S, Haldar SN, Soneja M, et al. Post COVID-19 sequelae: A prospective observational study from Northern India. Drug Discov Ther. 2021 Nov 21;15(5):254-60.
- Gamberini L, Mazzoli CA, Prediletto I, et al. Health-related quality of life profiles, trajectories, persistent symptoms and pulmonary function one year after ICU discharge in invasively ventilated COVID-19 patients, a prospective follow-up study. Respir Med. 2021 Nov-Dec;189:106665.
- Haddad A, Janda A, Renk H, et al. Long COVID symptoms in exposed and infected children, adolescents and their parents one year after SARS-CoV-2 infection: A prospective observational cohort study. EBioMedicine. 2022 Oct;84:104245.
- Franco JVA, Garegnani LI, Oltra GV, et al. Long-Term Health Symptoms and Sequelae Following SARS-CoV-2 Infection: An Evidence Map. Int J Environ Res Public Health. 2022 Aug 11;19(16):9915.
- Fernández-de-Las-Peñas C, Palacios-Ceña D, Gómez-Mayordomo V, et al. Fatigue and Dyspnoea as Main Persistent Pos-COVID-19 Symptoms in Previously Hospitalized Patients: Related Functional Limitations and Disability. Respiration. 2022;101(2):132-41.
- Garcia-Azorin D, Layos-Romero A, Porta-Etessam J, et al. Pos-COVID-19 persistent headache: A multicentric 9-months follow-up study of 905 patients. Cephalalgia. 2022 Jul;42(8):804-9.
- Lai CC, Hsu CK, Yen MY, et al. Long COVID: An inevitable sequela of SARS-CoV-2 infection. J Microbiol Immunol Infect. 2023 Feb;56(1):1-9.
- Chippa V, Aleem A, Anjum F. Post Acute Coronavirus (COVID-19) Syndrome. 2023 Feb 3.
- Arjun MC, Singh AK, Roy P, et al. Long COVID following Omicron wave in Eastern India-A retrospective cohort study. J Med Virol. 2023 Jan;95(1):e28214.
- Oronsky B, Larson C, Hammond TC, et al. A Review of Persistent Pos-COVID Syndrome (PPCS). Clin Rev Allergy Immunol. 2023 Feb;64(1):66-74.
- Davis HE, McCorkell L, Vogel JM, et al. Long COVID: major findings, mechanisms and recommendations. Nat Rev Microbiol. 2023 Mar;21(3):133-46.
- Szabo S, Zayachkivska O, Hussain A, et al. What is really 'Long COVID'? Inflammopharmacology. 2023 Mar 25:1-7.
- Mizrahi B, Sudry T, Flaks-Manov N, et al. Long covid outcomes at one year after mild SARS-CoV-2 infection: nationwide cohort study. BMJ. 2023 Jan 11;380:e072529.
- Baimukhamedov C. How long is long COVID. Int J Rheum Dis. 2023 Feb;26(2):190-2.
- Zanini G, Selleri V, Roncati L, et al. Vascular "Long COVID": A New Vessel Disease? Angiology. 2023 Jan 18:33197231153204.
- Carbone RG, Puppo F. Pericarditis in long COVID-19. Int J Cardiol. 2023 Apr 1;376:156.
- Liao B, Deng YK, Zeng M, et al. Long-term Consequences of COVID-19: Chemosensory Disorders. Curr Allergy Asthma Rep. 2023 Feb;23(2):111-9.
- The Lancet. Long COVID: 3 years in. Lancet. 2023 Mar 11;401(10379):795.