During the COVID pandemic, it was speculated that patients with the virus who were smoking-related might have a lower likelihood of disease exacerbation or death. To assess whether there is an association between smoking and risk of in-hospital mortality, SAVANA's big data and Natural Language Processing (NLP) technology is used.
MethodA retrospective, observational, non-interventional cohort study was conducted based on real-life data extracted from medical records throughout Castilla La Mancha using Natural Language Processing and Artificial Intelligence techniques developed by SAVANA. The study covered the entire population of this region with Electronic Medical Records in SESCAM presenting with a diagnosis of COVID from March 1, 2020 to February 28, 2021.
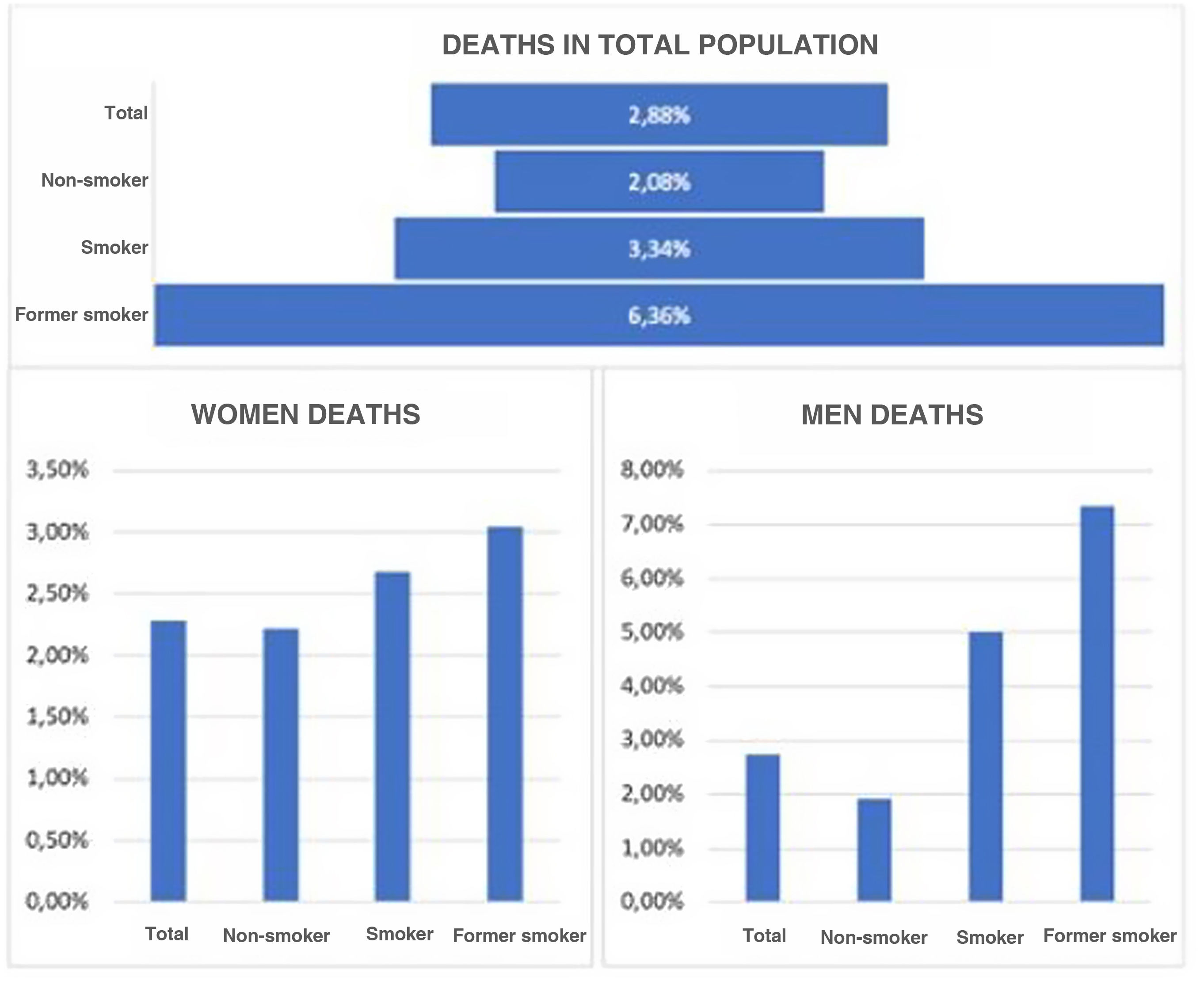
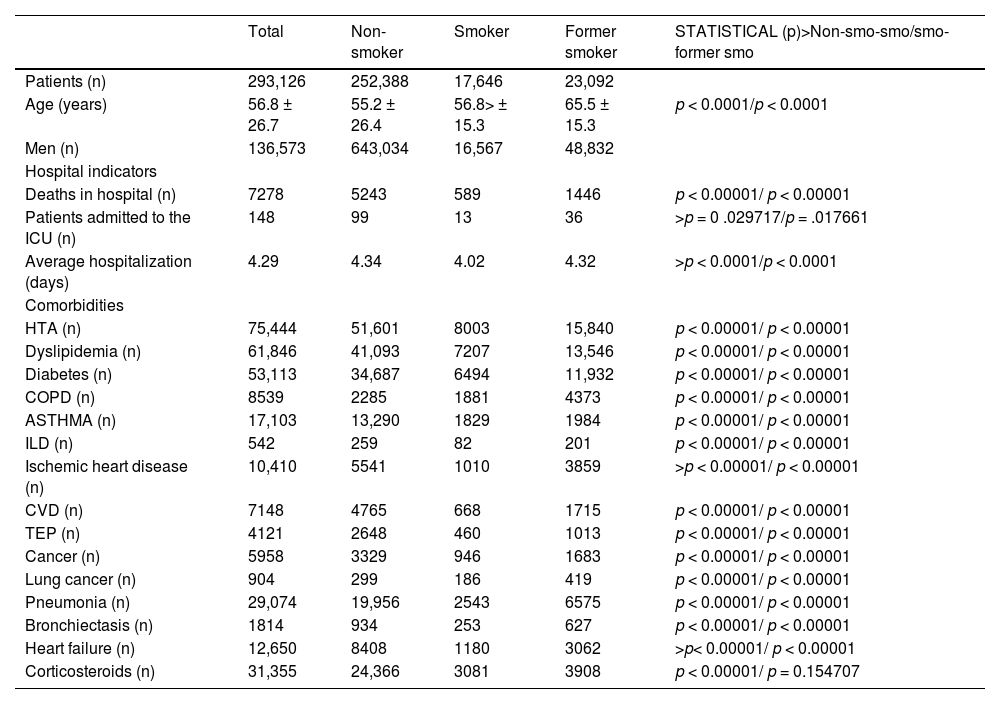
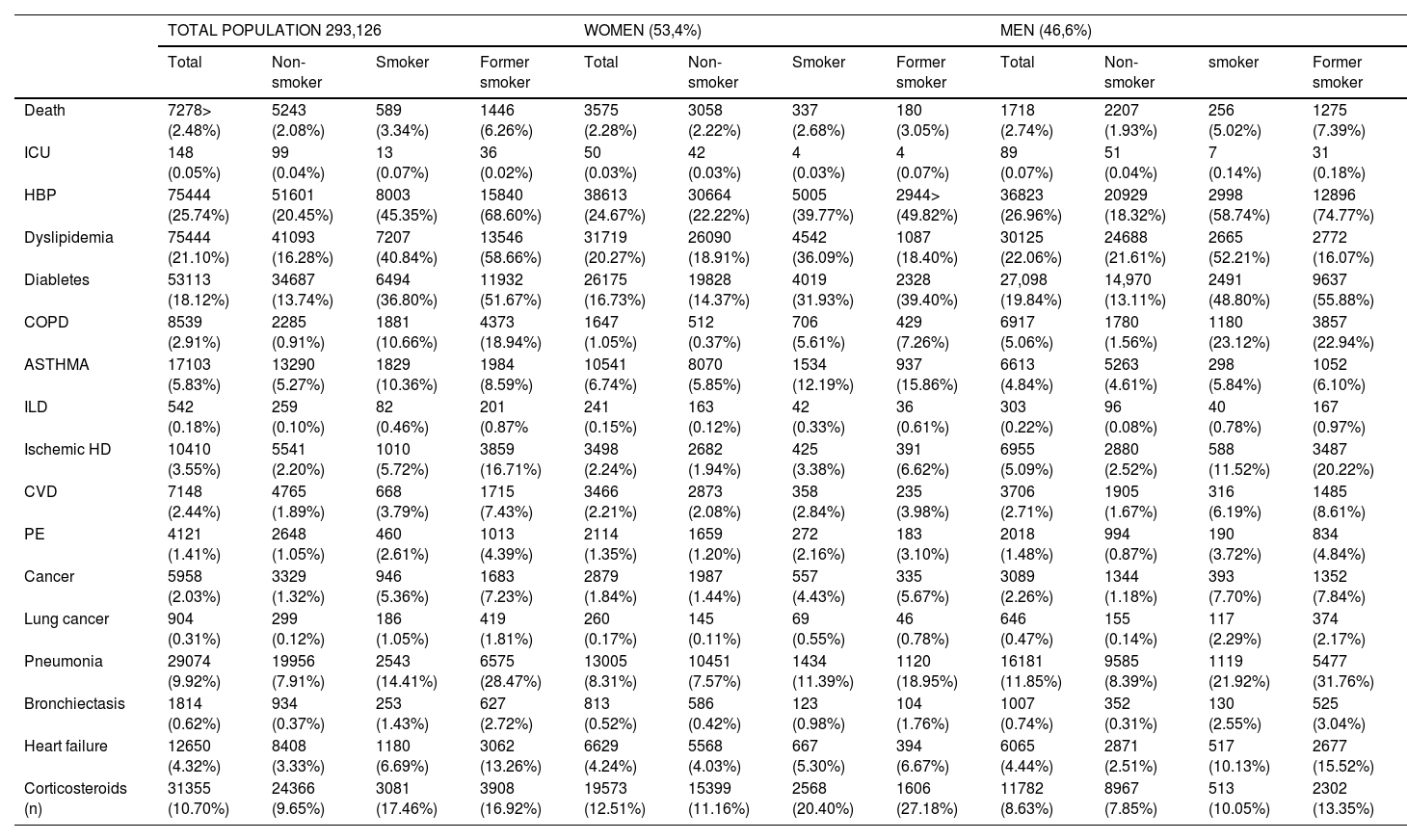
ResultsSmokers had a significantly higher percentage of cardiovascular risk factors (hypertension, dyslipidemia and diabetes), COPD, asthma, IDP, IC, CVD, PTE, cancer in general and lung cancer in particular, bronchiectasis, heart failure and a history of pneumonia (p < 0.0001).Former smokers, current smokers and non-smokers have a significant age difference. As for in-hospital deaths, they were more frequent in the case of ex-smokers, followed by smokers and then non-smokers (p < 0.0001).
ConclusionThere is an increased risk of dying in hospital in SARS-COV2-infected patients who are active smokers or have smoked in the past.
Durante la pandemia de COVID se especuló que los pacientes con el virus que tenían relación con el tabaco podrían tener una menor probabilidad de agravamiento de la enfermedad o muerte. Para evaluar si existe una asociación entre el tabaquismo y el riesgo de mortalidad intrahospitalaria, se utiliza la tecnología de big data y Procesamiento del Lenguaje Natural (PLN) de SAVANA.
MétodoSe llevó a cabo un estudio de cohortes retrospectivo, observacional y sin intervención basado en datos de vida real extraídos de registros médicos de toda Castilla La Mancha utilizando las técnicas de Procesamiento del Lenguaje Natural e Inteligencia Artificial desarrolladas por SAVANA. El estudio abarcó toda la población de esta Comunidad con Historia Clínica Electrónica en SESCAM que presentara diagnóstico de COVID desde el 1 de marzo de 2020 al 28 de febrero de 2021.
ResultadosLos fumadores tienen mayor porcentaje de factores de riesgo cardiovascular (hipertensión arterial, dislipemia y diabetes), EPOC, asma, EPID, CI, ECV, TEP, cáncer en general y cáncer de pulmón en particular, bronquiectasias, insuficiencia cardíaca y antecedentes de neumonía, de forma significativa (p < 0,0001). Los pacientes ex-fumadores, fumadores y no fumadores tienen una diferencia de edad significativa. En cuanto a las muertes hospitalarias, fueron más frecuentes en el caso de los exfumadores, siguiendo los fumadores y luego los no fumadores (p < 0.0001).
ConclusiónExiste un mayor riesgo de mortalidad intrahospitalaria en los pacientes infectados por SARS-COV2 y que sean fumadores activos o hayan fumado en el pasado.
Article
Diríjase desde aquí a la web de la >>>FESEMI<<< e inicie sesión mediante el formulario que se encuentra en la barra superior, pulsando sobre el candado.

Una vez autentificado, en la misma web de FESEMI, en el menú superior, elija la opción deseada.

>>>FESEMI<<<